Acceleration of blood flow through the carotid arteries. The norm of the diameter of the vertebral arteries
Table 1. Differential Diagnosis stenosis, angiospasm and arteriovenous malformation.
Feature name |
angiospasm |
||
Doppler spectrum: high frequency - low frequency - |
Frequency spread Significantly buffed |
Not changed |
Venous type |
Noise characteristic: high frequency - low frequency - |
Expressed Expressed |
Expressed Moderate |
Expressed Missing |
Circulatory resistance index (RI) |
|||
Pulsation Index (PI) |
|||
Cerebral reactivity |
Saved (reduced) |
Saved (reduced) |
Dramatically reduced |
Autoregulatory response |
Saved (lowered) |
Saved (lowered) |
Sharply reduced (absent) |
Dynamics of changes in blood flow (BFC) |
Missing |
Changes in time |
Missing |
The accuracy of diagnosis when using Dopplerographic features according to the literature is from 85 to 93%.
IV. Transcranial dopplerography
1982 is the starting point for transcranial dopplerography (R. Aaslid), which made it possible to diagnose intracranial lesions of the brachiocephalic arteries.
The method of transcranial dopplerography (TCD) is used to study blood flow in the arteries that form the large arterial circle (circle of Willis): intracranial sections of the ICA: middle, anterior and posterior cerebral arteries; ophthalmic artery, basilar artery and intracranial divisions of the vertebral artery.
The first stage of the study is to determine the location of the acoustic "window" through which the ultrasonic beam can penetrate with minimal energy loss. The main condition is the choice of successful sounding and the position of the sensor to obtain the optimal signal.
Three main pathways for the location of intracranial arteries have been described:
- 1. Temporal window (study of SMA, PMA, ZMA).
- 2. Orbital window (siphon of the internal carotid artery and ophthalmic artery).
- 3. Suboccipital window (main or basilar artery and intracranial segments vertebral arteries).
Location in the temporal region is carried out through the scales temporal bone. In older patients, the thickness of the bones or their density is so altered that it is sometimes difficult to obtain reliable signals due to the reduction in acoustic permeability. In all cases, the probe should be moved slowly, in small steps, paying attention to good ultrasonic contact between the probe and the skin, for which a sufficient layer of gel is applied.
Temporal windows located above the zygomatic arch. There are three positions of the temporal window:
- - the anterior window is located above the proximal part of the zygomatic arch;
- - the rear window is located in front of the ear. In some cases, this window is above the others;
- - the middle window is located between the front and rear windows, in the hair growth zone.
The criteria for identifying SMA are:
a) the blood flow is located at a depth of 55-65 mm.
b) the direction of blood flow to the sensor.
c) the signal responds with reduction or weakening during compression of the homolateral CCA.
Criteria for PMA identification:
a) the blood flow is located at a depth of 65-70 mm.
b) the direction of blood flow from the sensor.
c) the reaction of blood flow in the ACA during compression of the CCA depends on the presence or absence of the function of the anterior communicating artery (ACA). In most cases, the direction of blood flow in the ACA changes with compression of the homolateral CCA to the opposite when the ACA is functional. In the absence of PSA function, compression of the CCA leads to a reduction in blood flow in the ACA.
Criteria for identifying ZMA:
a) the blood flow is located at a depth of 65-75 mm.
b) the blood flow in the proximal segment of the PCA is directed towards the sensor and may have a bidirectional spectrum. In the distal segments of the PCA, blood flow is recorded with the direction from the sensor.
c) compression of the sibling CCA causes an increase in blood flow in the PCA when the PCA is consistent, or there are no changes.
Orbital window
When scanning through the orbital window, it is necessary to reduce the radiation power of the sensor to 10-20% to eliminate the damaging effect on the retina and lens of the eye. The sensor is placed on the closed eyelid, liberally lubricated with gel. This allows good ultrasonic contact without excessive pressure on the eye. The ICA siphon is located through the orbital window at a depth of 60-70 mm. The direction of blood flow is antegrade (toward the transducer).
The location of the ophthalmic artery is carried out through the orbital window at a depth of 30-45 mm; normally, antegrade blood flow is recorded, which has a characteristic pulsed waveform. Not a single intracranial vessel is found at this depth.
Suboccipital window
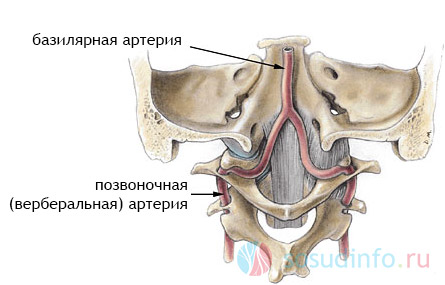
The acoustic accessibility of this window depends on the patient's posture: tilting the head forward, while the patient lies on his stomach or sits on a chair. Blood flow parameters in the intracranial vertebral arteries and in the basilar artery are examined through the suboccipital window. At a depth of 60 mm, the vertebral artery is located, while the sensor is located laterally relative to the sagittal plane. The direction of blood flow from the sensor.
The location of the basilar artery (BA) is carried out at a depth of 80-120 mm, the sensor is placed strictly along middle line at the point between the spinous process of the C2 vertebra and the edge of the occipital bone, at an angle of less than 30 degrees and the direction of blood flow in the OA is retrograde (from the sensor).
Tables 2 and 3 present the average values of the linear velocity of blood flow and indices, depending on the age according to the MAH.
Table 2. Normal performance blood flow according to MAH at the extracranial level (cm/sec) (Nikitin Yu.M. 1989).
LSC avg. |
LSK diast. |
SBI(%) |
||||
Table 3. Normal parameters of blood flow during transcranial study of MAH (cm/sec) (Nikitin Yu.N.).
SIPHON VSA |
||||||||
V. Changes in hemodynamic parameters in lesions vascular system according to dopplerography.
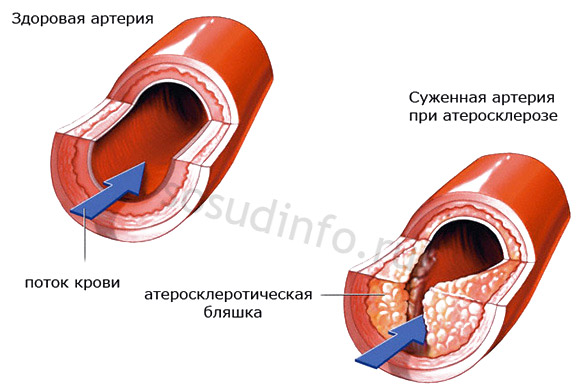
5.1. Diagnosis of stenosis of the common carotid artery.
In the 1970s, the method of "spectral analysis" of the Doppler spectrum was proposed, which made it possible to quantify the degree of stenosis of the common carotid arteries.
When the obstacle is less than 30% reduction of the lumen by the diameter of local hemodynamic shifts is not observed. Characterized by:
- - a slight increase in the spectral expansion index due to moderate flow turbulence;
- - a slight increase in the systolic maximum frequency compared with the corresponding artery;
- - a small spread of the systolic peak;
- - the signal in the pre- and post-stenotic zones is not changed.
With this degree of stenosis, the blood supply to the brain is kept sufficient for its normal functioning.
Signs of arterial stenosis up to 50%:
- - in the place of the obstacle and directly behind it, the linear velocity of blood flow increases significantly;
- - scatter of the high frequency spectrum;
- - the index of circulatory resistance increases in the prestenotic and stenotic zones;
- - the index of the spectral expansion increases, the complete filling of the spectral window;
- - concentration of the power spectrum of the systolic phase in the areas of medium frequencies;
- - high "whistling" noise;
- - in the distal part of the vessel, the blood flow is leveled off, with virtually no decrease in the linear velocity of blood flow;
- - distal to the obstacle, the value of the index of peripheral resistance may decrease.
With this degree of stenosis, reversible dysfunction of the central nervous system under increased loads.
Signs of arterial stenosis from 50 to 75%:
- - a pronounced increase in the maximum systolic frequency;
- - the shape of the Doppler curve is deformed due to a decrease in the diastolic component;
- - pronounced scatter of the high frequency spectrum;
- - the spectral window is absent due to the appearance of low-speed components of the spectrum;
- - concentration of the power spectrum of the systolic phase in the region of medium and especially low frequencies;
- - the appearance of a low-frequency spectrum of the systolic phase below the baseline;
- - increased index of circulatory resistance in the prestenotic and stenotic zones;
- - decrease in the maximum systolic frequency and index of circulatory resistance in the post-stenotic zone;
- - over the place of stenosis whistling sound, rough low-frequency noise, cut off.
This is a hemodynamically significant stenosis, manifested by a decrease in local blood flow to a critical level, with the possibility of developing focal symptoms under adverse conditions.
With high degrees of stenosis (more than 75%), “subtotal stenosis”:
- - a pronounced decrease in the maximum systolic frequency in the prestenotic and stenotic zones;
- - systolic and diastolic blood flow velocities have values that are hardly distinguishable in absolute value, the so-called “stenotic wall” appears,
- - registered spectral components under the zero line;
- - power concentration of the spectrum of the systolic phase in the low frequency region above and below the baseline;
- - the top of the curve is fuzzy, damped;
- - increased spectral expansion index, no spectral window;
- - an increase in the index of circulatory resistance in the prestenotic and stenotic zones;
- - a pronounced decrease in the maximum systolic frequency and circulatory resistance index in the post-stenotic zone;
- - pathological sound phenomena - damping, stuttering, grinding, rough low-frequency noise;
- - in the distal part of the vessel, the linear and volumetric blood flow velocity are reduced, the spectral filling is shifted to the low-velocity region of the spectrum, the peripheral resistance indices are reduced;
- - combined defeat of several MAGs.
With this degree of stenosis, a decrease in blood flow occurs below a critical level, and in the absence of adequate collateral circulation, local cerebral ischemia develops.
5.2. Diagnosis of stenosis of the internal carotid artery.
In the pathology of the carotid arteries, particular importance is given to hemodynamic disturbances in the supratrochlear arteries (SAA) - either retrograde blood flow, or biphasic, or pronounced asymmetry of blood flow in the SAA in a unilateral process.
With stenosis of the ICA, two variants of blood flow in the supratrochlear artery are possible:
1. Retrograde blood flow in the supratrochlear artery. The compression test of the homolateral CCA leads to a reduction or decrease in blood flow in the supratrochlear artery, or its inversion to antegrade. The presence of retrograde blood flow in the supratrochlear artery with ICA stenosis indicates its undoubted hemodynamic significance (more than 75%).
2. Antegrade reduced blood flow with asymmetry compared to the opposite supratrochlear artery more than 30%(with unilateral lesion of the ICA), a decrease in blood flow in the supratrochlear artery to 12 cm/sec or less with stenosis of both ICAs and the inability to use the asymmetry criterion.
The compression test of the CCA on the part of the study (reduction or decrease in blood flow in the supratrochlear artery) indicates the filling of the internal carotid artery from the system of the common carotid artery of the same name. As a rule, the combination of these criteria corresponds to hemodynamically insignificant stenosis (up to 75%) of the ICA in the extracranial segment.
Diagnosis of ICA stenoses is based on identifying patterns of obstructed perfusion in the prewall segments of the CCA and ICA; residual blood flow in the MCA on the side of the lesion. The phenomena of difficult perfusion, as well as the flow deficit above the affected area, are observed in hemodynamically significant lesions - IV-V degree stenoses: more than 75%. According to the classification of stenosis by degree, 5 options are distinguished: I - stenosis up to 40%, II - 40-60%, III - 60-75%, IV - 75-90%, V> 90%. Approximately determine the degree of stenosis allows the calculation of the Arbelli index (spectral expansion index), the values of which are close to the true severity of vasoconstriction. To determine the RFI, it is necessary to use continuous wave (CW) sensors.
With CCA stenoses, the deficit of blood flow in the MCA does not exceed 15%, which is explained by the satisfactory functioning of the collateral blood supply pathways. Stenosis of the ICA I-III degree with a functioning anterior communicating artery (PSoA) does not cause a shortage of blood flow in the MCA on the side of the lesion. With IV degree LBF in 40% is reduced by 25-35%; at the V degree, the LSC deficiency in 100% of cases exceeds 25%. Multiple stenosing lesions of cerebral vessels are observed according to the literature in 42% of cases. At the same time, the phenomenon of blood flow deficiency in both MCAs is less than 50% and is not symmetrical.
5 .3. Diagnosis of stenosis of the vertebral artery.
Stenosis of the vertebral artery may be suspected with blood flow asymmetry of more than 30% (for unilateral lesions). A decrease in the average blood flow velocity to 2–10 cm/sec undoubtedly indicates the presence of VA stenosis (extravasal compression or tortuosity). With bilateral VA stenosis, one has to focus only on absolute indicators of blood flow velocity. At the site of stenosis - an increase in the linear velocity of blood flow, mostly systolic, an increase in the systolic-diastolic ratio and an increase in the peripheral resistance index. With severe VA stenosis, the disappearance of the diastolic component to the baseline. The top of the Dopplerogram is rounded and “ragged”, the disappearance of the “plateau”, the shift of the maximum of the spectral power to the low-frequency region and the spread of the spectral power below the baseline, the reduction of the spectral “window”. A whistling sound is heard during VA stenosis.
For the final differentiation of changes in PA, a test with head turns should be performed. With an increase in blood flow velocity in PA, it speaks in favor of vertebrogenic effects. It is also necessary to locate the intracranial segments of the VA with a 2 MHz sensor - a decrease in the blood flow velocity along the VA in the V4 segment (up to the residual flow - a pronounced reduction in the systolic peak) makes it possible to diagnose VA stenosis in the proximal sections.
Stenoses less than 50% of the lumen do not cause perceptible changes in the Dopplerogram. The absence of pronounced stenosis of the contralateral VA stenosis of one VA does not cause significant hemodynamic changes in the arteries of the vertebrobasilar basin.
VA stenosis is differentiated from VA hypoplasia, in which the linear velocity of blood flow also decreases, but other Doppler parameters do not change, and when VA is located at the intracranial level, these same changes persist.
5 .four. Signs of stenosis subclavian artery(PCA).
Signs of proximal stenosis: asymmetry of the linear velocity of blood flow in the subclavian and axillary arteries by more than 30%. On the dopplerogram of the RCA, the disappearance of negative teeth; latent or transient subclavian steal syndrome; positive reactive hyperemia test. If subclavian steal syndrome is suspected, a reactive hyperemia test is performed. Using a sphygmomanometer cuff, compression of the shoulder is performed for 1.5-2 minutes (raising the pressure in the cuff to numbers exceeding the systolic blood pressure in the brachial artery by 20-30 mm Hg) followed by rapid decompression. Normally, the blood flow does not change ( negative test). If after decompression of the shoulder there is an accelerated blood flow through the VA, this is a positive test of reactive hyperemia, and the increased blood flow has a retrograde direction. There are three types of subclavian steal syndrome: constant(with occlusion of the RCA or the mouth of the VA) - the blood flow in the VA is constantly in a retrograde direction, increasing when performing a reactive hyperemia test; transient(with severe stenosis of the mouth of the RCA or the mouth of the VA) - retrograde blood flow along the VA in systole, and antegrade blood flow in diastole, and a positive test result - latent(with moderate stenosis of the RCA mouth or VA mouth) - antegrade blood flow in the VA at rest, a positive test result.
5 .5. Stenosis of the middle cerebral artery(SMA).
Stenosis of the MCA are characterized, in addition to the similar changes described above, by signs of activation of the collateral blood supply to its pool through pial anastomoses from the pools of the ACA and PCA, which is manifested by an increase in the linear velocity of blood flow in these vessels against the background of a decrease in peripheral resistance. Critical stenoses of the MCA, as well as the ICA, are characterized by a resonant oscillation of the vascular wall, which is manifested by a monotonous sound, as applied to cerebral vasospasm - “mur-mur”.
In cases of ICA occlusions with a non-functioning PSA, the flow in the MCA, as a rule, is not recorded or has minimal values, the flow deficit exceeds 80%.
5 .6. Stenosis and occlusion of the main artery.
Diagnosis of stenosis of the main artery possible only with TKD. The main criterion is a sharp increase in blood flow in an isolated area and an increase in peripheral resistance. At high degrees of stenosis, a symmetrical decrease in blood flow in the VA at the extra- and intracranial levels is possible with an increase in peripheral resistance indices. There may be a compensatory increase in blood flow along the ICA on both sides.
Occlusion OA characterized by the absence of blood flow distal to the site of occlusion, or collateral filling of the OA from the PCA. A pronounced symmetrical decrease in blood flow in the PA at the extra- and intracranial level with an increase in peripheral resistance indices. In the presence of PCA, blood flow in the P1 segment of the PCA can be directed towards the affected OA.
VI. Functional features systems cerebral circulation
Main Feature cerebral blood supply- collateral circulation. The value of collateral circulation in providing compensatory processes in the vascular system of the brain is extremely high. A rich network of anastomoses between the arteries that supply the brain with blood opens up great opportunities for the redistribution of blood between different areas of its vascular system. Normally, the anastomoses of the vascular system function with a certain frequency, depending on the real needs of the brain at one time or another. They are used to ensure blood flow to that basin of the brain, the blood supply of which has deteriorated due to any temporary restrictions on blood flow in the adductor vessel, which has arisen, for example, as a result of turning the head or hyperextension of the neck with compression of one of the main arteries of the head. It leads to sharp decline pressure in it, and after that - to the flow of blood through the arteries of the circle of Willis in the direction of a suddenly reduced pressure. Thus, the most important basal anastomosis, the circle of Willis, acts as a blood redistributor.
The inclusion of mechanisms of collateral circulation occurs with stenosis or thrombosis of the arteries of the brain and is the most important link in compensation.
There are four levels of collateral circulation:
- - extracranial;
- - on the basis of the brain;
- - on the surface of the brain;
- - intracerebral.
Extracranial anastomosis provides collateral circulation between the supratrochlear and supraorbital arteries - the terminal branches of the ophthalmic artery and represents the ophthalmic anastomosis.
Anastomosis extra-intracranial - between the muscular branches of the VA and the branches of the occipital artery - branches of the ECA. There is also an anastomosis between the superior thyroid artery from the ECA and the inferior thyroid artery, a branch of the subclavian artery.
The second level of collateral circulation is the great arterial circle, which is the main collateral collector of the brain. The advantage of anastomoses such as the circle of Willis is that when they are turned on, it does not take a long time to form the paths of collateral circulation, thus, the latter are a mechanism “quick” compensation of hemodynamic disturbances.
Cortical and intracerebral anastomoses have a much lower compensatory value for collateral hemodynamics.
When extracranial MAs (OCA, ICA) are affected, collateral circulation is most often realized through the anterior circle of Willis (through the ACA) and the posterior circle of Willis (PCA).
The inclusion of the ophthalmic anastomosis occurs with functional insufficiency of the circle of Willis or with bilateral occlusion of the internal carotid arteries.
Variants of collateral circulation in lesions of the main arteries are diverse, depending on the individual features of the structure of the circle of Willis and the localization of the brain lesion, which must be taken into account when interpreting Doppler ultrasound data.
VII. Atultrasonic doppler examination lower extremities.
7 .one. Dopplerografiya of arteries of the lower extremities.
Method doppler ultrasound arteries of the lower extremities is based on the registration of the ultrasound Doppler signal of blood flow velocity, the analysis of sound signals and the measurement of segmental blood pressure. The study is carried out in the patient at rest, in the supine position with the location of the blood flow in femoral artery(BA), posterior and anterior tibial artery (PTA) (PTA), arteries of the dorsal foot (ATS) and on the abdomen when registering the blood flow of the popliteal artery (PA). 4 MHz sensors are used for insonation of BA, PA and 8 MHz - for ZBA, PBA and ATS. The sensor is installed in the projection of the anatomical location of the artery or at the point of maximum pulsation at an angle of approximately 45o to the skin surface. The flow characterization is based on an estimate of the shape of the curve. Normally, the blood flow through the arteries of the upper and lower extremities is of the main type.
Most important characteristic waveform of blood flow is a peak in systole, reflecting the magnitude and nature of the translational blood flow. In peripheral arteries, the systolic peak is normally sharp, high, and well defined. A decrease in amplitude, distortion of the peak shape in the form of expansion, splitting or rounding indicates the presence of an obstruction to blood flow proximal to the point under study.
The end of the systolic peak is immediately replaced by a period of significant reverse blood flow at the beginning of diastole. The severity of reverse blood flow in early diastole is defined as the value arterial pulse and peripheral resistance. The presence of reverse blood flow indicates normal patency of the arteries proximal to the point under study. The absence of reverse flow pulsation at the beginning of diastole is an important ultrasound sign of an occlusive arterial lesion.
From the middle to the end of diastole in the form of a wave of blood flow, one or more waves of blood flow are usually observed, which are a reflection of the elasticity of the arterial wall. Smoothing or disappearance of fluctuations at the end of diastole suggests a decrease in elasticity, but may also indicate an occlusive lesion located more proximally.
With stenosis located proximal to the location point, a single-phase pulsation is detected with expansion, splitting of the systolic peak and the absence of reverse blood flow in early diastole. An audio signal is determined with a weakened first component and smoothness of the second and third peaks, since the blood flow velocity is reduced. The described changes characterize magistral-variable type of blood flow.
As the occlusive process progresses, further changes in the waveform occur. In critical stenosis or occlusion, the blood flow in the proximal segment is characterized by a smoothed pulsation, a decrease and rounding of the systolic peak, and a slow rise and fall of the blood flow curve. The more pronounced the lesion, the worse the collateral circulation and more changes are observed on the blood flow curve. By ear, a continuous, low-frequency sound of low intensity is determined. The picture described is typical for collateral type of blood flow in the studied artery.
Blood flow peak values are used to quantify the blood flow waveform. When interpreting absolute values, it is necessary to take into account the level of systemic blood pressure and the value of cardiac output.
A semi-quantitative assessment of the form of blood flow is carried out using a number of calculated indices:
- - pulsator index (PI) is the ratio of the sum of the peak rates of direct and reverse blood flow to the average speed. Normally, PI exceeds 5.5 for BOTH and increases in value in the distal direction. Its value does not depend on the angle between the direction of the ultrasound beam and the vessel.
- - Damping - factor or damping factor (DF) - reveals, as well as PI, an occlusive lesion in peripheral arteries. DF is calculated as the ratio of distal to proximal PI. For example, DF1=PI BOTH/PI of the brachial artery. Normal values DF lie in the range of 1.15-1.48 and do not change throughout the arterial bed of the limb.
Thus, blood flow analysis is based on a qualitative assessment of the waveform and its derivatives, i.e. calculated indices. Characteristic features development of an occlusive lesion are: a change in the shape and size of the systolic peak, the disappearance of a wave of reverse blood flow, a decrease in PI less than 4 and DF less than 1.
Measurement of blood pressure.
The study is carried out in the supine position. First, the blood pressure on the shoulder is measured at the location of the blood flow in the radial artery. A prerequisite is the measurement of blood pressure in both arms. Measurement of blood pressure in the lower extremities is performed at 4 levels: ankle and top part lower leg, lower and upper third of the thigh. The size of the pneumatic cuff must correspond to the size of the limb, its width must be 40% of the circumference of the limb, otherwise incorrect results may be obtained. Segmental pressure is determined for each level of the limb by monitoring the blood flow signal. The location of the blood flow is performed on the ZBA or ATS. In cases where it is impossible to determine the blood flow in these arteries, the blood flow in the VA is located to measure the pressure on the thigh. Note that systolic BP is the pressure in the artery located under the cuff, and not in the artery where the blood flow is located.
In healthy individuals, the pressure measured in the upper third of the thigh exceeds the pressure on the shoulder by 20-30 mm Hg. Art., and at the level of the ankle is approaching or slightly higher than the systemic. In occlusive lesions of the arteries, reduced blood flow to the limb leads to local hypotension. The fall in ankle systolic pressure is proportional to the degree of arterial lesion. Thus, ischemic pain at rest is usually associated with systolic pressure at the ankle less than 40 mm Hg. Art.
A variant of the norm is considered to be a pressure difference of less than 20 mm Hg. Art. between limbs at the same level. The pressure gradient between adjacent levels of blood pressure measurement normally does not exceed 30 mm Hg. Art. The difference is more than 30 mm Hg. Art. considered as a sign reflecting occlusion or severe stenosis of the arteries between these segments.
Measurement results can be expressed not only as absolute values, but also in the form of indices. Ankle-brachial index or ankle pressure index (LIP) is calculated as the ratio of ankle blood pressure to upper arm blood pressure. A LID value of less than 1.0 indicates the presence of an occlusive lesion in the arteries of the limb. In general, in limbs with occlusion or critical stenosis at one level, LID is more than 0.5, and with lesions at several levels, less than 0.5. The LID value makes it possible to assess the degree of development of collateral circulation and the functional state of the arteries of the lower extremities. LID values up to 0.7 indicate an occlusive lesion of the artery with CC in the compensation stage; from 0.7 to 0.4 - in the stage of subcompensation, a decrease in LID less than 0.4 indicates decompensation of blood circulation. The severity of ischemia of the lower limb, which develops with occlusive damage to the arteries, depends on the location, number of storeys, degree of damage, and the state of the distal bed. However, the main factor determining the clinical picture of the disease is the degree of development of CC. Note that the decrease in LID correlates with the degree of ischemia of the lower extremities. So, at the first degree, the LID values vary within 0.8-1.0, at the second degree - 0.6-0.8, at the third degree - 0.4-0.6, and at the fourth - less than 0.4 .
Thus, the measurement of systolic blood pressure at the ankle level with the calculation of LID is a reliable criterion in assessing the arterial blood flow of the lower limb. A LID value of less than 1.0, firstly, indicates the development of a hemodynamically significant occlusive lesion in the arteries of the lower limb, and secondly, it allows assessing the level of collateral circulation and the functional state of the arteries of the studied limb. However, LID does not allow localization of the lesion. Measurement of segmental systolic blood pressure in the limb gives Additional information about the location of the lesion.
Clinical examination of patients with damage to the arteries of the lower extremities should begin with questioning and examination of the extremities.
There is a classification of Pokrovsky-Fonten, depending on the severity of ischemic pain syndrome in the lower extremities, according to which 4 stages of occlusive lesions are distinguished:
Stage I (functional compensation) - pain in the lower extremities appears only with a large physical activity, for example, when walking a distance of more than 1 km, cramps or paresthesias appear in the lower extremities after a long stay of more than 1 hour in a static position, coldness of the legs is noted;
II (subcompensation) - pain appears when walking a shorter distance; if the patient can walk more than 200 m without pain with a normal step, the severity of ischemia corresponds to stage IIA, if pain occurs when walking less than 200 m - stage II B, also trophic disorders (muscle hypotrophy, dry skin, brittle nails, cracks skin on the foot) and coldness of the lower extremities, chilliness (socks are worn even in summer)
III (decompensation) - pain is observed at rest or when walking less than 25 m; neuritis joins, due to ischemia, swelling of the lower extremities, cyanosis, lymphadenitis;
IV (destructive changes) - there are ulcerative-necrotic changes in the tissues, pronounced edema of the lower extremities.
Table 4. Normal blood flow velocities in the arteries of the lower extremities.
Vmax (cm/s) |
V diast. (cm/sec) |
|
7 .2. Ultrasound technique for examining the veins of the lower extremities.
The veins of the lower extremities are divided into superficial, lying in the subcutaneous tissue and deep, accompanying the arteries of the same name. Both venous systems anastomose with each other.
Superficial venous system. It is formed by the great saphenous vein (GSV) and the small saphenous vein (SSV).
The GSV, being a continuation of the medial marginal vein of the foot, begins anterior to the medial malleolus, follows up the medial edge of the tibia, passes to the antero-medial surface of the thigh and flows into the common femoral vein (CFV).
MSV is formed from the lateral marginal vein of the foot, rises along the posterolateral surface of the lower leg and flows into the popliteal vein (PCV) in the region of the popliteal fossa.
deep venous system The confluence of the dorsal and plantar veins forms paired posterior and anterior tibial and peroneal veins, which, in turn, merge to form the PCV.
The popliteal vein, located in the popliteal fossa posteriorly and laterally from the popliteal artery, goes up and passes into the femoral vein (FV). BV accompanies the superficial femoral artery (SFA) along the lower 2/3 of the thigh. In the upper third of the thigh, the BV merges with the deep femoral vein (TFV), which accompanies the artery of the same name, and becomes the common femoral vein (CFV).
OBV, suppressing the inguinal fold, becomes the external iliac vein (IVC), which, after joining with the internal iliac vein, forms the common iliac vein (OPV).
The inferior vena cava is the confluence of the right and left OPV.
The connection between the superficial and deep venous systems, mainly on the lower leg and, to a lesser extent, in the thigh area, is carried out by perforating veins, which under normal conditions shunt blood from the superficial venous system into the deep The obturating process in the deep venous system, as well as dysfunction of the venous valves of the perforating veins, leads to pathological shunting of blood from the deep venous system to the superficial one, the development of varicose veins, venous hypertension, and trophic changes in the tissues of the lower extremities.
Femoral vein:
The 4 MHz transducer is located in the area of the inguinal ligament just medial to the signal from the femoral artery.
To assess the viability of the valves, functional tests are carried out:
- 1. Valsalva test used to assess the function of the valvular apparatus, mainly large veins of the lower extremities. The principle of the maneuver is as follows: when inhaling in healthy individuals, venous blood flow decreases significantly, and when holding the breath and straining on the lower abdomen, it completely stops and the maximum noise during the subsequent exhalation. Valvular insufficiency is indicated by a retrograde straining wave with a peak velocity of approximately 30 cm/s and a duration of more than 1 second, or a slower but longer wave.
- 2. Distal compression is used to assess the patency of the studied area of the vascular system. Alternately produce compression below the location of the sensor. Normally, with distal compression, an increase in the velocity of antegrade blood flow in the vein by 2 times or more is detected. When scoring the femoral artery, compression of the thigh, lower leg and dorsoreflexion of the foot are performed alternately.
- 3. Proximal compressions are performed to assess the state of the valvular apparatus of the popliteal veins and veins of the leg and are evaluated similarly to the Valsalva test. The sensor is located below the compression point. Normally, proximal compression should not cause changes in the venous signal (since unchanged valves allow blood to flow only in the proximal direction). In the presence of even a subclinical lesion of the valvular apparatus, proximal compression causes an increase in phlebonoise, which indicates blood flow regurgitation.
Literature
- 1. Gaidar B.V., Dudanov I.P., Parfenov V.E., Svistov D.V. //Ultrasonic research methods in the diagnosis of lesions of the aortic branches. Petrozavodsk. 1994. - 70 p.
- 2. Dadvani S.A., Ternovoy S.K., Sinitsin V.E., Artyukhina E.G. //Non-invasive diagnostic methods in surgery abdominal cavity and arteries of the lower extremities. M.: Vidar, 2000. - 139 p.
- 3. K clinical guide to ultrasound diagnostics. T. IV / edited by Mitkov V.V. M.: Vidar, 1997. - 338 p.
- 4. Kulikov V.P. //Color duplex scanning in diagnostics vascular diseases. Novosibirsk, 1997. - 155 p.
- 5. Lelyuk V.G., Lelyuk S.E. //Ultrasonic angiology. M.: real time, 2003. 322 p.
- 6. Nikitin Yu.M. //Physical principles of ultrasonic dopplerography: Reference manual/ CJSC “Spectromed”, 1995.- 21 p.
- 7. Guide for physicians // Clinical ultrasound diagnostics of lower extremity vein pathology. Ed. Yu. V. Novikova. Association “Russian Doppler Club”. Kostroma: DiAr, 1999.-72 p.
- 8. Sinelnikov R.D., Sinelnikov Ya.R. “Atlas of human anatomy”, volume 3. M. Medicine, 1992.- 232 p.
- 9. Educational guidance // Doppler ultrasound in the diagnosis of occlusive lesions of the arteries of the brain and extremities. Scientific Center for Cardiovascular Surgery. A. N. Bakuleva RAMS. M., 1996.- 72 p.
- 10. Shakhnovich A.R., V.A. Shakhnovich //Diagnosis of disorders of cerebral circulation. Transcranial dopplerography. M., Association of Book Publishers 1996. - 446 p.
- 11. Shakhnovich V.A. //Cerebral ischemia. Neurosonology. M., 2002. - 306 p.
you can read about vertebral artery syndrome
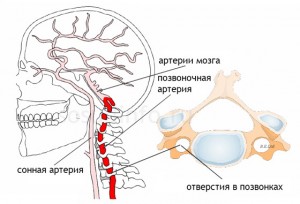
As you know, the vertebral arteries depart from the subclavian arteries in the upper part chest cavity, pass through the openings of the transverse processes of the cervical vertebrae, then enter the cranial cavity, where they merge into a single basilar artery located in the lower part of the brain stem. Branches depart from the basilar artery, providing blood supply to the brain stem, cerebellum and occipital lobes of the cerebral hemispheres. Vertebrobasilar insufficiency, or vertebral artery syndrome, is a condition in which blood flow in the vertebral and basilar arteries is reduced. The cause of these disorders may be extravasal compression, increased tone of the vertebral artery (arterial discirculation, vegetative-vascular dystonia), atherosclerosis, anatomical features buildings, etc. Violations of volumetric and linear blood flow velocities in the vertebral arteries associated with extravascular compression can be detected both on one and both sides. The most common compressive factor is muscle tissue, which is associated with the anatomical localization of the vertebral arteries. Compression of the vertebral arteries is also possible with bone tissue (osteophytes, hernia intervertebral disc, subluxation of the cervical vertebrae, etc.).
Diagnosis of vertebral artery syndrome (or vertebrobasilar insufficiency) is carried out using doppler ultrasound; modern combined systems, including dopplerography and duplex scanning, allow assessing the state of the vertebral arteries. With ultrasound examination of the vessels of the head and neck, including the vertebral arteries, using linear sensors with a frequency of 7.5 MHz or more (scanning along the anterior and lateral surfaces of the neck), it is possible to conduct a qualitative and quantitative (spectral analysis) assessment of blood flow in the vessels. Qualitative analysis includes an assessment of the diameter (the norm is 2.8-3.8 mm) and the shape of the vessel (the presence of bends, loops, etc.). When conducting a standard spectral analysis of the vertebral arteries, they measure (most often in the intervals between II, III and V, VI cervical vertebrae) systolic (normal - 31-51 cm / s), average (normal - 15-26 cm / s), diastolic ( normal - 9-16 cm / s) and volumetric (normal 60-125 ml / min) speed, as well as pulse (normal - 1.1-2.0) and resistant (normal - 0.63-0.77) impulses . However, with osteochondrosis of the cervical spine, osteophytosis, instability of the vertebrae, herniated intervertebral discs, when conducting an ultrasound scan of the vessels of the head and neck in a standard position and when conducting positional tests (turns and tilts of the head, various hand movements in shoulder joint) the vessel can be pinched to one degree or another, which will be reflected in a change in the ultrasonic signal with a deviation from the norm above the considered indicators.
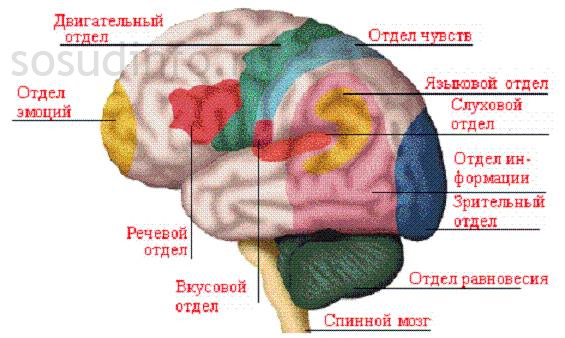
The core of the clinical picture of vertebral artery syndrome is a symptom complex, which includes seven main groups of signs: (1) headache, (2) cochleovestibular dysfunction, (3) visual disturbances, (4) pharyngeal and (5) laryngeal symptoms, (6) vegetative-vascular dystonia, and (7) asthenic syndrome. Consider clinical features visual disorders (more precisely, the pathology visual analyzer) with vertebrobasilar insufficiency as part of the vertebral artery syndrome.
The close connection between the pathology of the brain and the eye is due to the anatomical and functional unity of their blood circulation. The vertebral arteries, being the first branch of the subclavian arteries, form the main artery, constituting the vertebrobasilar system that feeds the occipital lobes of the cerebral cortex with the central link of the visual analyzer and the brain stem with the nuclei and conductors of the oculomotor, trochlear and abducent nerves and the system of the posterior longitudinal bundle. Anatomical studies(G.D. Zarubey, 1966) clarified the existence of two systems that feed the optic nerve - peripheral, represented by the choroid plexuses of the soft meninges, and central, to which most authors refer the central artery of the optic nerve, which, according to some researchers, is a branch of the ophthalmic artery, according to others, a branch of the central retinal artery. outflow venous blood occurs mainly through the central vein of the retina and the vein of the choroid plexus of the pia mater.
In the foreign literature there are a number of works devoted to the clinic of visual disturbances in occlusions of the intra- and extracranial parts of the vertebral arteries (Synonds, Mackenzie, 1957; Hoyt, 1959; Minor et al., 1959; Kearns, 1960). Unfortunately, in the observations of these authors clinical diagnosis not always confirmed instrumental methods research. It is believed that visual disorders are caused by ischemia of the cortex of the occipital lobes, especially their poles and areas adjacent to the spur groove. With careful questioning, they are detected in almost all patients with vertebrobasilar insufficiency of any etiology. Visual disturbances can be transient or persistent. Photopsies are transient. Patients complain about the appearance before the eyes of "black flies", "soot", "sparks", "lightning", multi-colored and golden dots that seem to flicker and oscillate. Photopsies in cases of cerebral circulation disorders are pinpoint, their occurrence is not associated with a light source, they continue even with closed eyes. Such patients often note "blurring" of vision in both eyes, blurred images. With a sharp change in the position of the head, these phenomena increase, there is also a deterioration general condition, the appearance or intensification of headache, dizziness. After such an attack, vision can be fully restored. These phenomena may long precede the development of other symptoms of vertebrobasilar insufficiency. Sometimes these phenomena, along with dizziness, are provoked by tipping the head back, and in some cases appear against the background of excessive physical or emotional stress. More complex photopsies have also been noted, for example in the form of "white shiny rings", often shiny zigzag lines. Periodically, photopsies were observed in the form of a moving stream of multi-colored (red, yellow and green) cubes. In all cases, the visual disturbances are transient and last only a few seconds. Blurred vision of objects in the form of sensations of a veil or fog before the eyes is noted, according to the literature, in about half of the patients. These phenomena often occur against the background of fatigue: during long walking over rough terrain or during physical work associated with holding the breath, sometimes when reading, or develop after fainting. Visual disturbances were included by J. Barre (1926) as an obligate symptom of the posterior cervical sympathetic syndrome. Well-known function changes optic nerves with irritation of the sympathetic plexus of the carotid artery. With vertebral artery syndrome, visual disturbances such as flickering scotomas, fog before the eyes, pain in the eye, photophobia, lacrimation, a feeling of sand in the eyes, and changes in pressure in the arteries of the retina are described. A.M. Grinshtein (1957), G.N. Grigoriev (1969), as well as D.I. Antonov (1970) pointed to occasional attacks of unilateral loss of the field of vision or part of it, combined with spasm of the retinal artery in case of damage to the cervical sympathetic structures. Sometimes there is redness of the conjunctiva. The dependence of visual disturbances on the pathology of the spine is evidenced by a change in the state of the fundus at the time of stretching of the cervical spine. During stretching according to Bertshi or during extension of the neck (Popelyansky Ya.Yu.), some of the subjects also noted changes in the fundus, expressed by the expansion of large veins, narrowing of the arterial trunks; there were also cases of expansion of the retinal arteries with a constant caliber of the veins. In conclusion, it should be noted that in the syndrome of the vertebral artery (vertebrobasilar insufficiency), such short-term violations of higher cortical functions as different kinds(!) visual agnosia (with impaired optical-spatial perception) as a result of ischemia in the distal cortical branches of the posterior cerebral artery.
Hypoplasia of the vertebral artery is a pathological condition manifested by impaired blood supply different zones brain and changes in general hemodynamics in the body. The disease develops as a result of a congenital defect and a change in the diameter of the vessels.
What is hypoplasia?
Hypoplasia is characterized by intrauterine underdevelopment of tissues or organs. Incomplete development of the vertebral (vertebral) artery is manifested by a narrowing of its diameter. Hypoplasia can be bilateral or unilateral (right or left). The most common is hypoplasia of the right vertebral artery.
Due to the intracranial segment of the vertebral artery, the basilar artery is formed, giving rise to the posterior cerebral arterial vessels, which are part of the arterial circle of Willis and form the vertebrobasilar basin. Vessels of the vertebrobasilar basin provide blood supply posterior regions brain (cerebellum, medulla, cervical segment spinal cord), which suffer as a result of a violation of normal hemodynamics.
Causes of the disease
Underdevelopment of blood vessels occurs as a result of exposure to the body of the pregnant woman and the fetus:
- medicines;
- infectious diseases;
- bad habits;
- ionizing radiation;
- toxic substances.
It may also be the result genetic predisposition to vascular disease. 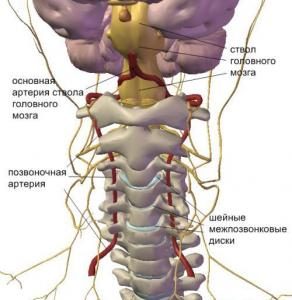
The disease rarely manifests itself in childhood, but can occur with a critical narrowing of the lumen of the artery and dissociation of the circle of Willis. Most often, middle-aged and older people are affected. Pathology may not manifest itself due to the compensatory abilities of the body:
- the development of collaterals and additional anastomoses of the vertebral artery as a result of the formation of which, less developed branches of the blood vessel take on part of the load and temporarily provide normal blood supply;
- an increase in blood pressure develops secondarily and temporarily facilitates the flow of blood under pressure to the brain through a narrowed blood supply vessel.
Often, hypoplasia of the vertebral arteries can occur against the background of other diseases:
- osteochondrosis of the cervical segment of the spine and its complications;
- spondylolisthesis (displacement of the vertebrae);
- atherosclerotic vascular lesions;
- the formation of a thrombus in the lumen of the affected blood vessel.
Symptoms and consequences
Signs of hypoplasia of the vertebral artery are very diverse and depend on the degree of damage. Often, due to the similarity of symptoms, the disease is not diagnosed for a long time, and various neurological diagnoses are erroneously made. The symptoms of the disease can vary and directly depend on the area of the brain where the blood supply is difficult.
Main features:
- Frequent dizziness, possible fainting.
- Prolonged headaches, migraines.
- Lethargy, drowsiness.
- Drops in blood pressure.
- Decreased visual acuity.
- Noise in the ears, hearing loss.
- Decreased memory and concentration.
- Cerebellar disturbances: instability when walking, impaired fine motor skills.
- Weakness in the arms and legs, numbness, change in sensitivity.
- Rarely movement disorders in the form of paresis and paralysis.
Hypoplasia of the left vertebral artery in general clinical symptoms differs little from damage to the right vertebral artery. Focal neurological symptoms of vascular disorders may change slightly. Persistent vertebrobasilar insufficiency due to hypoplasia leads to transient ischemic attacks, ischemic strokes of varying severity, cerebellar infarction.
Diagnostics

Vascular insufficiency can be diagnosed using:
- angiography of the vertebral arteries and all vascular structures of the brain;
- ultrasound examination of the vessels of the neck and head;
- magnetic resonance imaging of the head and neck with contrast.
These research methods allow you to determine the intensity of blood flow and evaluate the diameter of the arteries. Normally, the diameter of the vertebral artery is about 3.6-3.9 mm; if a decrease in diameter of less than 3 mm is detected, hypoplasia is confirmed.
Treatment
Depending on the intensity of cerebrovascular accident in the vertebrobasilar region, conservative or surgical treatment is prescribed.
Conservative treatment based on application medications and is symptomatic. The following drugs are used:
- cerebral vasodilators (trental, vinpocetine, agapurine) provide the expansion of cerebral vessels and improve microcirculation;
- antihypertensives contribute to the normalization of blood pressure;
- antiplatelet agents (aspirin, dipyridamole) prevent the formation of blood clots;
- nootropics (cerebrolysin, glycine, piracetam, phezam) improve metabolic processes in the brain.
Painkillers, antiemetics, antidepressants, sleeping pills are also symptomatically prescribed. Conservative treatment does not eliminate vascular hypoplasia, but with slight hypoplasia of the vertebral arteries, it improves cerebral circulation and avoids surgical intervention.
Surgery
With segmental stenosis, limited occlusion of the vertebral artery and pronounced signs of vertebrobasilar insufficiency, the following is performed:
- balloon angioplasty is a method of endovascular intervention under X-ray control. A conductor is inserted into the lumen of the peripheral artery, through which a balloon catheter is passed to the site of stenosis. After the balloon has been inflated and the diameter of the artery expanded, the balloon catheter is withdrawn;
- stenting of the vertebral artery - before the introduction of the stent, balloon angioplasty is performed, and then, to maintain the patency of the artery, a frame metal stent is installed, which firmly fixes vascular wall, preventing possible re-narrowing of the lumen.
Frequent headaches, dizziness, a feeling of heaviness in the occipital region, tinnitus are complaints that are most often made by patients with vertebrobasilar insufficiency. In more severe cases, there is a violation of speech and swallowing, vision, drop attacks (a sudden fall of the patient, not accompanied by loss of consciousness and the appearance of warning symptoms). If these important symptoms do not pay attention in time, it is possible to develop an ischemic stroke, especially in people over 40-45 years old. It has been established that stroke occurs within 5 years in 30% of patients with symptoms of vertebrobasilar insufficiency. Screening instrumental methods for detecting circulatory disorders in the vertebral arteries are: rheoencephalography (REG) - a non-invasive study of cerebral blood flow, allows you to assess disorders of the vascular system caused by atherosclerosis, hypertension, identify changes in intracranial venous circulation and patency disorders in the vertebrobasilar vascular system, as well as ultrasound duplex scanning main vessels head and neck. Specialists of the Kazan City Polyclinic No. 11 medical institution carry out these techniques to study cerebral blood flow, which made it possible to raise the diagnostic and treatment process to a qualitatively new level.
The syndrome of circulatory insufficiency in the vertebrobasilar system has formed as an independent clinical concept in the 50s of the XX century, during the period of revision of views on the pathogenesis of ischemic disorders of cerebral circulation and the formation of the concept of the leading role in this mechanism of vascular brain failure. Time put everything in its place and determined a worthy, but more modest position for this pathogenetic (hemodynamic) subtype of cerebral ischemia among a number of others. Thus, ischemic disorders of cerebral circulation in this vascular system, different in their origin and mechanisms of development, began to be considered from the general standpoint of their heterogeneity.
At the same time, the peculiarities of the structure and functions of this arterial system, which provides the vital structures of the brain, and the peculiarity of clinical symptoms during discirculation in it, led to its isolation in latest version international classification into an independent symptom complex - "syndrome of the vertebrobasilar arterial system" within the framework of "transient transient cerebral ischemic attacks (attacks) and related syndromes" (ICD-X, G 45.0).
Brief functional-anatomical and clinical-physiological characteristics. The vertebrobasilar system (VBS) supplies blood to one third of the brain. It covers its departments, which differ significantly both in structural and functional terms. These are the cervical spinal cord, the brain stem and cerebellum, part of the thalamus and the hypothalamic region, partially occipital, parietal and mediobasal regions. temporal lobes brain. With insufficient blood supply, symptoms are observed in it in various combinations. However, within the framework of clinical polymorphism, it is possible to distinguish groups of characteristic symptom complexes, which will be discussed below.
The peculiarities of the extracranial parts of the VBS include the location of the vertebral arteries in the openings of the bone canal of the transverse processes of the cervical vertebrae, which are easily displaced relative to each other during movements of the head and neck. In addition, they are closely adjacent to the vertebral bodies. In this case, even under normal physiological conditions, there is compression and restriction of blood flow in one or both arteries. Normally, blood circulation in them is usually not disturbed due to sufficient compensatory capabilities. The position changes with hypoplasia or atherosclerotic stenosis of the arteries. Then extravasal factors (compression by articular processes in case of instability of the cervical spine or osteophytes in uncovertebral areas, etc.) become decisive in the genesis of circulatory failure in the IBS. Compression of the vertebral arteries is also possible by the neck muscles (scalene, long neck, inferior oblique muscle of the head) when they contract at certain head positions. The role of congenital and acquired deformities of the initial section of these arteries with the formation of septal stenoses, sharply and suddenly limiting blood flow with a vivid clinical picture, usually vestibular disorders, has been proven.
Underestimation of the factor of extravasal compressions and the role of deformities extracranial departments vertebral arteries is one of the most common diagnostic errors and the cause of unsuccessful drug treatment circulatory insufficiency in the VBS. Adding to its symptoms a characteristic clinical "vertebral artery syndrome" with severe pain and angiodystonic signs requires a systematic examination of the atlanto-occipital region, cervical spine and extracranial parts of the vertebral arteries for targeted treatment.
The greatest success of ultrasound in the diagnosis of vascular pathology was achieved at the end of the last century, when devices operating in duplex mode appeared. Only a few years ago, triplex Dopplerography began to be used, which allows for a three-dimensional reconstruction of any vessel in “real time”. Modern devices for ultrasound diagnostics of the highest and expert class allow visualizing vessels with a diameter of less than 1 mm, determining pathological changes in them or surrounding tissues. This is very important when examining patients with vertebral artery syndrome. As is known, the vertebral arteries depart from the subclavian arteries in the upper part of the chest cavity, pass through the foramina of the transverse processes of the cervical vertebrae, then enter the cranial cavity, where they merge into a single basilar artery located in the lower part of the brain stem. Branches depart from the basilar artery, providing blood supply to the brain stem, cerebellum and occipital lobes of the cerebral hemispheres. Vertebrobasilar insufficiency, or vertebral artery syndrome, is a condition in which blood flow in the vertebral and basilar arteries is reduced. The cause of these disorders can be extravasal compression, increased tone of the vertebral artery (arterial dyscirculation, vegetative-vascular dystonia), atherosclerosis, anatomical features of the structure, etc. Violations of volumetric and linear blood flow velocities in the vertebral arteries associated with extravasal compression can be detected as on one or both sides. The most common compressive factor is muscle tissue, which is associated with the anatomical localization of the vertebral arteries. Compression of the vertebral arteries is also possible with bone tissue (osteophytes, herniated disc, subluxation of the cervical vertebrae, etc.).
Determination of localization and possible cause compression of the vertebral artery contributes to targeted therapeutic or surgical intervention in order to normalize blood circulation.
The value of the method is that the study is carried out not only in the stationary position of the patient lying on his back, but also using numerous functional positional tests. In a standard study, linear sensors with a frequency of 7.5 MHz or more are used, scanning along the anterior and lateral surfaces of the neck. At the same time, a qualitative and quantitative (spectral analysis) assessment of blood flow in the vessels is carried out. Qualitative analysis includes an assessment of the diameter (the norm is 2.8-3.8 mm) and the shape of the vessel (the presence of bends, loops, etc.). When conducting a standard spectral analysis of the vertebral arteries, they measure (most often in the interval between the V and VI cervical vertebrae) systolic (normal - 31-51 cm / s), average (normal - 15-26 cm / s), diastolic (normal - 9- 16 cm / s) and volumetric (norm 60-125 ml / min) speed, as well as pulse (norm - 1.1-2.0) and resistance (norm - 0.63-0.77) impulses.
However, with such pathological conditions such as osteochondrosis of the cervical spine, instability of the vertebrae, herniated discs, when performing a triplex scan of the vessels of the head and neck in the standard position, the patency of the vertebral arteries may not be impaired. At the same time, during positional tests (turns and tilts of the head, various movements of the arms in the shoulder joint), the vessel can be pinched to one degree or another, which will be reflected in a change in the ultrasound signal. Thus, this technique makes it possible to detect the presence of not only static, but also “hidden” compression of the vertebral arteries.
The information obtained during these tests allows the doctor to determine several important points: location and cause pathological process, the degree of violation of the patency of the vessel, changes in blood flow under the influence of various factors, including pharmacological tests. Taking into account the peculiarities of dynamic compression of the vertebral artery due to the pathology of the cervical spine helps to determine the optimal volume and technique of surgical intervention - extravasal decompression of the vessel, which makes it possible to achieve best results in the treatment of vertebral artery syndrome.
Operations, receptions can be carried out under the control of ultrasound manual therapy, massage. This technique allows you to evaluate the effectiveness of the chosen method of treatment, if necessary, adjust the treatment regimen.
For the period from 2009 to 2010. we have passed 614 ultrasound examinations of the extracranial part of the main arteries of the head. All studies were carried out on an ultrasound scanner LODIG 3 PRO using a linear probe and 228 studies of rheoencephalography on a 6-channel multifunctional computer rheograph REO-spectrum-3 by Neurosoft. Main value of our research is non-invasiveness in determining the state of cerebral blood flow, which makes it possible to study volumetric pulse blood filling in the main vascular basins, to assess the tone of vessels of various sizes and the state of venous hemodynamics, to carry out the production of functional tests and individual selection of drugs.
Intravascular obstruction is the most common finding in our studies. Atherosclerotic lesions of the brachiocephalic arteries various localizations and degrees of severity found in 42% of the patients examined by us. Of these, hemodynamically significant stenoses were found in 61% of patients, which corresponds to the contingent of those examined. Among those examined, 72% were patients over 60 years of age.
The second most common cause of hemodynamic disturbances in the arteries of the brachiocephalic zone among the patients examined by us is a violation of the normal course of the vessels. This applies to the arteries of the carotid and vertebrobasilar basins. We have identified crimps of various shapes: C-shaped, S-shaped, knee-shaped, and finally, loop-shaped. Violation of hemodynamics in case of tortuosity of vessels was observed, as a rule, in the presence of an acute angle in the place of inflection of the vessel. Hemodynamically significant tortuosity is manifested by varying degrees of turbulence, as well as an increase in speed at the site of angulation.
Congenital malformations blood vessels(angiodysplasia, vascular malpharmacy) are the result of a genetically determined violation of the normal development of the vascular system in embryogenesis. Angiodysplasia in the form of hypoplasia is the most common malformation of blood vessels identified in our studies. According to our data, hypoplasia of the vertebral arteries is detected in about 18.9-19.2% of patients with pathology of the brachiocephalic arteries. Along with those named among the causes of circulatory failure in the vertebrobasilar system is extravascular obstruction - extravasal compression - frequency - 4% among the patients examined by us. Extravasal compression is associated with a violation of the lumen of the vessel by a process that acts on the vessel from the outside. These are cases of vessel compression by a tumor, hematoma, inflamed tissue, osteophytes, herniated disc.
Ultrasound duplex scanning of the extracranial part of the main arteries of the head, along with rheoencephalography, significantly expands the screening capabilities in the diagnosis of vertebral artery syndrome.
Kurbangaleev V M, Terentyeva L A,
MUZ "City Polyclinic No. 11", Kazan
Gimaeva S T.
Federal State Institution "Main Bureau of Medical and Social Expertise in the Republic of Tatarstan"
Hypoplasia of the vertebral artery: signs, treatment, consequences
Hypoplasia of the vertebral artery is most often a congenital defect, and can be either right-sided or left-sided. In the future, the disease leads to a violation of hemodynamics (circulation), which especially affects the posterior parts of the brain. Most often, this causes numerous dysfunctions in the work of the heart and circulatory system in general, the vestibular apparatus and other organs.
General information about hypoplasia
Full blood circulation in all parts of the brain is possible due to; it is formed from the right and left branches of the spinal arteries.
Under normal conditions, both the right and left vertebral arteries are equally developed. In the region of the subclavian artery towards the cranial cavity, they are divided into small vessels.
The term "hypoplasia" in medicine describes the underdevelopment of tissues or an organ; it can be both a congenital pathology and an acquired one.
Bilateral hypoplasia is much less common than right-sided or left-sided, although the latter case is already considered quite rare. But since the adaptive capabilities of the body are not unlimited, their depletion very quickly leads to the stage of decompensation and the need for surgical intervention.
Causes and consequences of the disease
How does hypoplasia develop?
Factors affecting the occurrence of hypoplasia affect human body still in the womb, however, the same can be said about most diseases and birth defects.
It is believed that the following processes and phenomena can cause hypoplasia:
- Bruises and various injuries of the mother during pregnancy;
- Abuse of some medicines, alcohol, nicotine, and drugs when carrying a child, poisonous chemical compounds can also give a similar effect;
- Infectious diseases of the expectant mother;
- Genetic predisposition to diseases of the circulatory system;
Hypoplasia of the vertebral arteries does not always develop due to the above situations, these cases only significantly increase the risk of pathologies in the development and functioning of the circulatory system. But sometimes, however, children with congenital hypoplasia are born in the absence of any of the listed reasons. So modern medical luminaries do not yet have a consensus on this matter, although there are many conflicting theories.
What threatens the occurrence of the disease in the future?
In some cases, the defect does not make itself felt until a certain period or even throughout life, since hemodynamic disturbances are attributed to other diseases or simply poor health, if the symptoms are not particularly pronounced.
The narrowing of the opening of the artery at the site of its confluence with the bone canal during hypoplasia significantly impedes the flow of blood to the brain tissues. The consequences of hypoplasia, therefore, can be unpredictable, and to identify real reason multiple dysfunctions in this case is not possible immediately. However, some of them do not pose a serious threat to health, but definitely worsen the quality of life. These include increased fatigue, periodic severe headaches, a decrease in visual acuity and hearing.
Symptoms and diagnosis of hypoplasia
Problem symptoms
The main characteristic of the disease is the variety of symptoms, which can vary significantly in each individual patient. This applies to both intensity pain and manifestations of underdevelopment of the vertebral arteries in general. In some cases, the patient learns about a possible diagnosis only when undergoing a planned medical examination, because the clinical picture very blurred, and the symptoms of hypoplasia are very similar to the external manifestations of other diseases.
It is possible to talk about the presence of hypoplasia of the right or left arteries if the following signs are present:
- Frequent causeless dizziness;
- Headaches of varying intensity;
- Distorted perception of the position of the body in space, which occurs suddenly;
- Dysfunctions of the nervous system;
- Violation or complete disappearance of sensitivity in certain areas (including limbs);
- Frequent high blood pressure.
Nonspecific signs of hypoplasia are the result of circulatory disorders in the body, but to identify them true reason quite difficult even for an experienced specialist. These include dizziness, accompanied by loss of consciousness, sudden disorientation in space due to a violation movement coordination, which can lead to falling, and staggering when walking or changing body position.
Loss of coordination of movements is a rare, but rather unpleasant manifestation of hypoplasia. This usually looks like an unreasonable fall or collision with people or objects, and the person himself may experience sensations similar to those that appear after a long ride on a carousel.

Usually, the intensity and frequency of all signs of hypoplasia of the vertebral arteries increases with the aging of the body, since age-related phenomena include a decrease in the elasticity of small and large vessels and their contamination. Thus, the lumen in the arteries affected by hypoplasia is additionally reduced, and hemodynamics worsens.
Identification of the disease
If there are suspicions, it will be useful to make an appointment with a neurologist. Examination of the patient and existing complaints about well-being are the reason for a more thorough check than the initial examination. If during the examination the specialist detects anomalies in cervical region, it's probably worth doing ultrasound procedure spinal arteries.
The result of ultrasound is a confirmation or refutation of a possible diagnosis. The conditional norm is the diameter of the lumen from 3.6 to 3.8 mm; vasoconstriction up to 2 mm is considered the main diagnostic sign. As an additional examination, the doctor may also recommend a pass, which, with the help of x-ray radiation and certain contrast agents allows you to accurately identify the condition of the blood vessels.
"Right" and "left" hypoplasia
Hypoplasia of the right vertebral artery
Most experts do not share the symptoms of right and left hypoplasia as specific when it comes to external manifestations illness.
A significant difference in symptoms is observed only in case of violation of some brain functions, since the branches of the subclavian artery feed its various departments. Thus, in various areas leads to different consequences. It is worth noting that the symptoms of hypoplasia of the right vertebral artery are almost always common.
In addition to the symptoms listed above, this pathology development of the circulatory system can cause emotional disorders. Patients often experience unreasonable mood swings with a high polarity of mood swings. Weakness and lethargy often occur even without overload and stress as such, and a depressed state can last for several days in a row. Complaints of increased fatigue and drowsiness occur in almost every patient, as well as a severe headache. occurs both with hypoplasia of the right and left vertebral arteries.
Hypersensitivity or total loss sensitivity of some parts of the body often indicates that the part of the brain responsible for a certain area suffers from poor blood flow. Sometimes this makes it possible to make the correct diagnosis or confirm the current one.
The main trouble in the pathology of the right vertebral artery are concomitant diseases, for which hypoplasia acts as a kind of catalyst for degenerative processes. One of these diseases is, which leads to additional circulatory disorders, since it significantly constricts blood vessels.
With hypoplasia of the right artery, a strong meteosensitivity may develop in the future, and sometimes there are problems with sleep.
The difference in the consequences of hypoplasia of the right and left vertebral arteries is explained by the fact that they feed different parts of the brain.
Hypoplasia of the left vertebral artery
Unlike the right one, hypoplasia of the left vertebral artery may not manifest itself immediately, but closer to adulthood, since the symptoms are associated with circulatory disorders.
Hemodynamic dysfunction manifests itself not only in the form of poor vascular patency and organ ischemia as a consequence, but also as stagnation of blood in others. This happens only after a sufficiently long period of time, since adaptation mechanisms can very effectively avoid problems in the work of the organism that develops due to a deterioration in blood flow for the time being. The clinical significance of symptoms increases with age-related changes in organs and tissues, and at the primary stages, attention should be paid to Special attention to some external manifestations.
Pain in the cervical spine is considered one of the most indicative signs of left artery hypoplasia, although in the absence of other symptoms it is impossible to make a correct diagnosis.
The appearance of connections between the branches of the main main vessels (vascular anastomoses) is a typical manifestation of the action of compensatory mechanisms in the underdevelopment of both vertebral arteries. The achieved effect is lost in case of deterioration of vascular patency due to concomitant diseases.
In the case of hypoplasia of the left artery, hypertension (increase in pressure) is a secondary disease, and, in fact, a mechanism for adapting the body to the existing state of affairs. Under high pressure, blood passes into the brain much more easily even through a hole of small diameter, since the lumen of the artery in the case of hypoplasia is much narrower.
Method of treatment of hypoplasia
Paradoxically, in certain cases, a person does not need treatment for vertebral artery hypoplasia, since the body's adaptive capabilities allow it to cope with hemodynamic disorders for a long time and prevent the appearance of clinical symptoms in principle, and the supply of blood to the brain does not deteriorate.
But if the signs of the disease have already shown themselves, then you should not delay a visit to the doctor, since vivid symptoms almost always indicate a rather serious problems with health. Most often this happens due to, with constant high physical and emotional stress, as well as in case of failures in the work of compensatory mechanisms.
Atherosclerosis, as well as stenoses of vessels of a different nature, is one of the main causes of hypoplasia. Therefore, in order to get rid of health problems, treatment should be comprehensive and exclude phenomena that painfully constrict blood vessels.
In this case, treatment of hypoplasia should be started as soon as possible in order to prevent a significant deterioration in well-being and, if possible, avoid surgery, although most often surgical intervention(for example, and/or ) is the only alternative, as the disease becomes severe.
With a relatively early diagnosis, specialists still try to avoid surgical intervention into the patient's body with drug therapy. Drugs and pressure lowering drugs are the mainstay of treatment, and are recommended as an adjuvant.
In addition to the above methods, other means modern medicine does not have, although some "alternative medicine centers" offer other procedures as therapy - acupuncture, massage, various gymnastic complexes. You should not unconditionally rely on the promises of people who most often do not even have a special education. If desired, and only after consultation with your doctor, you can combine both methods.
Video: stenosis of the mouth of the left vertebral artery. Angioplasty with stenting
