Middle cerebral artery of cerebral infarction. Blood supply to the brain
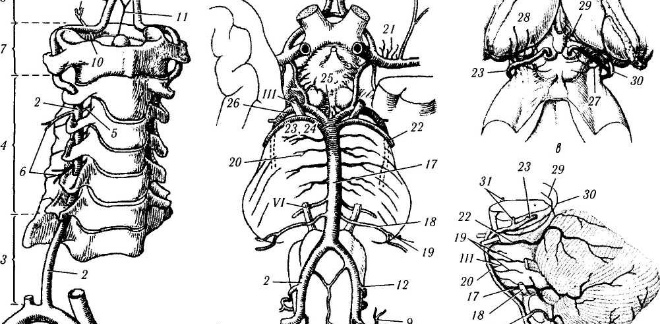
The middle cerebral artery, which is the main branch of the internal carotid artery, passes through the Sylvian sulcus (the artery of the Sylvian sulcus) and supplies a vast area on the convex surface and in the depths of the cerebral hemisphere. Branching of the middle cerebral artery is variable. It branches into:
a) deep, or central, branches extending from the initial section of the trunk of the middle cerebral artery, plunging into the medulla and supplying the region of the subcortical nodes;
b) cortical, or peripheral, arteries, of which the first departs from the beginning of the middle cerebral artery; they supply a significant part of the convex surface of the cerebral hemispheres.
B.V. Ognev divides the cortical arteries in turn into external ones, which originate from the outer semicircle of the middle cerebral artery and are distributed on the inner surface of the temporal lobe, internal, extending from the inner semicircle of the middle cerebral artery.
Among the cortical branches of the middle cerebral artery, the following stand out.
The fronto-orbital artery supplies the external and bottom surface frontal (upper frontal and most of the lower frontal gyrus), respectively, cytoarchitectonic fields 47, 46, 44 and partly exciting 11, 10, and also the anteroinferior part of the lower frontal gyrus. Together with the precentral artery, the fronto-orbital artery supplies blood to the base of the inferior frontal gyrus. There are anastomoses with branches of the anterior cerebral artery. Since the fronto-orbital artery sometimes consists of an inferior and an external branch, the symptoms of small-focal softenings are different (non-thrombotic softenings). With thrombosis of the artery trunk, the blood supply is turned off not only in the fronto-orbital, but also in the precentral, central and postcentral arteries and a violation of motor functions develops in the extremities opposite to the focus. When blood circulation is disturbed in the left fronto-orbital artery, motor aphasia occurs.
Precentral inferior artery(a. praecentralis inferior) feeds the region of the anterior central gyrus (lower part 6, lower and middle parts 4 and partially 43), the opercular region, the insular gyrus (islet), the lower part of the leg of the anterior central gyrus, the leg of the middle frontal gyrus and upper part peduncles of the inferior frontal gyrus. It has anastomoses with the anterior cerebral artery. With softening in the region of the precentral artery, phenomena of facio-brachial monoparesis develop on the opposite side, a violation of the masticatory muscles, and with left-sided localization of the focus - dysarthria, rarely motor aphasia.
Central (lower postcentral) artery (a. centralis or rolandica) supplies the region of the anterior and posterior central gyri, 4, 3, 2, 1, 40 (in the lower and middle parts) and 43. Softening in the area of vascularization of the central artery causes the appearance of paralysis or paresis, characterized by: a) the predominance of loss of function (the area of the cortical centers for the distal section is supplied from the anterior cerebral artery), b) a combination of movement disorders with muscle atrophy. With obliteration of the central artery, monoparesis or hemiparesis occurs. With the predominance of damage to the branches supplying the anterior and posterior central gyrus, movement disorders combined with sensory disorders, which, however, are never intense and have a limited character. In contrast to diffuse hemianesthesia in opposite limbs with capsular lesions, with cortical lesions, sensory disturbances are local in nature. If the opercular region is affected, swallowing and chewing disorders may develop.
The postcentral artery is described by B.V. Ognev and N. Metalnikova as a branch of the inferior parietal artery, which vascularizes the supramarginal gyrus, the lower and sometimes the posterior part of the superior parietal lobule, and the anterior superior occipital gyrus. When blood circulation is disturbed, unsharply expressed disorders of sensitivity occur.
The anterior, or ascending, parietal artery (a . parietalis interior s . ascendens) supplies the region of the parietal lobe corresponding to the cytoarchitectonic fields, partially subcortical white matter in the region of the supramarginal gyrus. With softening in the region of the artery, hemiparesis occurs with impaired sensitivity, stereognosis, a disorder of the body scheme, anosognosia (agnosia of the fingers, autotopagnosia), disorientation in time (the patient does not know the month, hour), apraxia in the left-sided focus) and atactic disorders. With blockage of the anterior parietal artery, a pseudo-thalamic syndrome is observed, which differs from the true thalamic syndrome in less severity of pain and greater preservation of sensitivity. With it, cortical hyperpathy, a disorder of deep sensitivity, impaired coordination, involuntary movements fingers (pseudo-athetotic movements), imitative synkinesis. The appearance of hyperpathy in pseudothalamic syndrome is due to pathological condition excitability of the thalamic thalamus as a result of a violation of the connection between the thalamus and the cortical section of the skin analyzer, while in true thalamic syndrome, hyperpathy occurs due to damage to the thalamic thalamus itself.
The posterior, or horizontal, parietal artery (a. parietalis posterior s. inferior, s. horisontalis) branches in the supramarginal gyrus, the lower section of the superior parietal lobule, sometimes captures the posterior section of the superior parietal lobule and the anterior superior occipital gyri and supplies the areas, respectively, 39 and partially 40 Brodman, back of a small patch of fields. With foci of softening caused by blockage of the posterior parietal artery, phenomena of agnosia and hemianopsia occur, and with left-sided foci, the phenomena of optical agnosia, alexia, aphasia.
The artery of the angular gyrus (a. angu is) departs from the middle cerebral artery in the final branch or is a continuation of the middle cerebral artery itself. It branches in the angular gyrus and the anterior part of the external occipital gyri, where it anastomoses with the branches of the posterior cerebral artery, which corresponds to cytoarchitectonic 39. When the artery of the angular gyrus is blocked on the left, constructive apraxia, alexia, agnosia, acalculia, and sensory aphasia occur.
The posterior temporal artery (a. temporalis posterior) branches in the posterior sections of the upper and middle temporal gyri and supplies the temporal artery, respectively, with cytoarchitectonic fields 21 ( middle part fields), 22 (middle part of the field), 37 (posterior half of the field) and 52, 42. In the presence of foci of softening, sensory or sometimes amnestic aphasia occurs. Thromboembolism of the posterior temporal artery is possible, as a result, sensory aphasia develops, the degree of which depends on the severity of collateral circulation (the possibility of blood supply to the affected from the anterior temporal artery, anastomosing with the posterior temporal artery).
The middle temporal artery (a. temporalis media) branches in the middle part of the upper and middle temporal gyrus and in the middle part of the lower temporal gyrus. Supplies the area corresponding to cytoarchitectonic fields 22 (anterior part of the field) and 21. Symptoms of defeat clearly do not come to light; sometimes unsharply expressed sensory disorders (sensory aphasia).
The anterior temporal artery (a. temporalis anterior) departs from the beginning of the trunk of the middle cerebral artery, branches in the anterior third of the superior and middle temporal gyri with spread into the superior temporal sulcus, with the exception of the temporal pole, and supplies the territory of the temporal, respectively, to fields 38 (posterior part of the field) and 20. B. V. Ognev N. Metalnikova, in contrast to Fua, three temporal arteries are distinguished, of which the middle temporal artery is unstable. L. Ya. Pines observed sensory aphasia and auditory agnosia in lesions of the anterior temporal artery.
The polar temporal artery (a. temporalis polaris) branches on the lower inner and outer surface of the temporal pole and supplies a small portion of the latter, respectively, to the cytoarchitectonic 38. Isolated does not cause a clear dysfunction.
The main area of vascularization of the middle cerebral artery is:
- the lateral part of the orbital surface of the frontal lobe, the insula and the entire convexital surface of the cerebral hemispheres, except for the strip vascularized from the anterior cerebral artery and the posterior region, including the occipital pole, vascularized from the posterior cerebral artery;
- upper half of the anterior and posterior femur of the internal capsule, optic fascia;
- caudate (except for the lower part of the frontal pole) and the lateral part of the globus pallidus.
In case of circulatory disorders in the middle cerebral artery, various clinical syndromes occur, depending on the location and nature pathological process. The symptomatology varies according to the lesion, depending on whether the blockage of the trunk or branches of the artery occurs.
Since Foix's time, it has been believed that complete and partial obstruction of the middle cerebral artery causes more severe lesions in the area closer to the obliteration than in the distant one. long-term observations have shown that with complete blockage of the trunk of the middle cerebral artery, blood circulation is disturbed mainly in nearby branches ( deep arteries), but in the distal branches it is less disturbed. Thus, with complete blockage of the trunk of the middle cerebral artery, a proximal type of blood supply shutdown develops in the arterial system. With partial blockage of the trunk of the middle cerebral artery or the internal carotid artery, a distal type of circulatory disorder may occur in the system of the middle cerebral artery. Partial blockage of the trunk of the middle cerebral artery (parietal thrombus, atherosclerotic plaque and causes non-thrombotic softening in the area of vascularization of the distal cortical branches of the middle cerebral artery. Ischemic non-
Since Foix's time, it has been believed that complete and partial obstruction of the middle cerebral artery causes more severe lesions in the area closer to the obliteration than in the distant one. long-term observations have shown that with complete blockage of the trunk of the middle cerebral artery, blood circulation is disturbed mainly in the nearby branches (deep arteries), while in the distal branches it is less disturbed. Thus, with complete blockage of the trunk of the middle cerebral artery, a proximal type of blood supply shutdown develops in the arterial system. With partial blockage of the trunk of the middle cerebral artery or the internal carotid artery, a distal type of circulatory disorder may occur in the system of the middle cerebral artery. Partial obstruction of the trunk of the middle cerebral artery (parietal thrombus, atherosclerotic plaque and causes non-thrombotic softening in the area of vascularization of the distal cortical branches of the middle cerebral artery. Ischemic necrosis develops as a result of reflex spasm and angioparesis of the distal branches.
Rapidly transient circulatory disorders in the basin of the middle cerebral artery, proceeding with the same type of symptoms, are caused by pathological impulses from the internal carotid artery and depend on the severity of thrombosis occlusion) of the internal carotid artery, morphological changes in the walls of the middle cerebral artery and the possibilities of compensating blood circulation from the circle of Willis.
Complete blockage of the trunk of the middle cerebral artery to the place where the deep branches originate causes extensive softening of the brain parenchyma, which is supplied by the branches of the middle cerebral artery. In such cases, coma occurs, hemiplegia develops (paralysis is more pronounced in the arm), cortical-type hemianesthesia, hemianopsia, gaze paresis, aphasia in the left-sided focus); the course is progressive, the outcome is sometimes fatal. 114-118 shows variants of softening in thrombosis of the middle cerebral artery and hemorrhage in its vascularization.
Incomplete blockage of the trunk of the middle cerebral artery in the initial section causes a violation of blood circulation in the deep branches, in the no-orbital artery, sometimes partially in other proximal outgoing arteries. softening develops in the region of the internal bag (the putameno-caudal part of the shell of the caudate body, the outer part of the pale nucleus, the outer bag, the fence, the insula, the posterior external part of the orbital and partially lower (third) frontal gyri. Semiotics of incomplete blockage of the trunk of the middle cerebral artery, accompanied by shutdown deep branches, is as follows: hemiplegia, evenly expressed in both extremities opposite to the focus, with persistent hypotension behind deep damage motor fibers in the inner bag and lesions of the striatal system. Slightly pronounced sensory disorders join the paralysis. Supranuclear lesion of the motor cranial nerves in such cases causes central paresis of the facial and hypoglossal nerves. With the localization of the focus in the left hemisphere, the phenomena of motor aphasia develop, which is sometimes replaced by persistent dysarthria.
Blockage of the middle cerebral artery after the departure of the deep branches near the ascending branch (a. ascendens) causes softening of the subcortical white matter (semioval center) in the posterior sections of the middle and lower frontal gyri, in the insula, in the anterior and posterior central gyri and the anterior parietal, sometimes in the superior temporal gyrus. Necrosis of the white matter extends deep into, sometimes reaching the ependyma of the lateral ventricle. The area of the brain supplied by the anterior parietal artery usually remains intact; blood circulation in the fronto-orbital artery, as well as in the posterior long cortical branches (posterior parietal, posterior temporal), suffers less. The insula is most deeply affected, and the subcortical white matter in the back of the anterior and posterior central gyri (semioval center).
The clinical picture is hemiplegia with hemianesthesia, impaired stereognosis, but without hemianopsia. Paralysis of the upper monoplegic extremities opposite to the focus is expressed unevenly: it is usually more affected than the leg. This is explained by the fact that paralysis is caused by damage to the centers in the brain and conductors in the white matter, and paralysis is caused by a violation of only conductive innervation (cortical centers are vascularized behind the anterior cerebral artery). In case of circulatory disorders in the left middle cerebral artery, aphasia, alexia, agraphia, acalculia, apraxia, agnosia develop. With an extensive focus, total aphasia, hemianopsia can be observed. blockage of the central part of the middle cerebral artery disrupts the blood flow in the deep (perforating) arteries, necrosis of the shell, caudate and internal capsule occurs. Mild striatal symptoms join hemiplegia.
Obstruction of the trunk of the middle cerebral artery in its distal section (after the ascending branch leaves) causes circulatory disturbance in the posterior parietal, posterior temporal, and angular arteries. Focal softening develops in the lower parietal lobule (field of the anterior part of the occipital (field in the posterior part of the upper and middle temporal gyri (fields 21), and the subcortical white matter is also destroyed up to the ependyma of the lateral ventricle, as well as visual pathways. With the lesion, a parietal-temporal-angular syndrome develops: hemianopsia caused by a lesion of the conduction system and characterized by a predominance in the lower quadrant. In the case of left-sided localization, sensory or amnesic aphasia, apraxia, and sometimes agnosia are also observed. With an extensive focus, symptoms of damage to the posterior central gyrus and fibers of the anterior central gyrus - hemiplegemianesthesia with a predominant violation of discriminatory sensitivity, a sense of localization, and stereognosis join the parietotemporal angular syndrome. With topical diagnosis, this syndrome differs from the syndrome caused by softening of the cortical branches of the middle cerebral artery, the phenomena of apraxia, sensory aphasia, sensory disturbances and hemianopsia.
The combination of lesions of the anterior and posterior parietal branches of the middle cerebral artery leads to the appearance of hemianesthesia and mild hemiplegia. When sensitivity is violated, especially discriminatory (a sense of localization, etc.), complex forms of sensitivity and stereognosis. Sometimes there is a violation of the body scheme, apraxia, imitation synkinesis appears. The clinical picture resembles the thalamic syndrome, but differs from the originality of sensory disorders (thalamic syndrome is dominated by violations of protopathic sensitivity) and a violation of higher cortical functions. circulatory disorders in the posterior temporal artery join the damage to the parietal arteries, then there are phenomena of sensory-amnestic aphasia.
With bilateral circulatory disorders in the middle cerebral artery and localization of foci in symmetrical areas of the brain, complex syndromes arise. The syndrome of bilateral circulatory disorders in the deep branches of the middle cerebral artery is characterized by the following phenomena: quadriparesis or quadriplegia, dysarthria, dysfunction of the pelvic organs, amimia, fine tremor or parkinsonian-type hyperkinesis. Sometimes there is a pronounced pseudobulbar syndrome with impaired speech, amimia, dysphagia, ataxia, gait change, tremor, hypotension in the presence of pyramidal paresis, reflexes of oral automatism, impaired urination, mental disorder.
With symmetrical bilateral foci in the striopallidar region, parkinsonism occurs with amimia, rigidity, increased postural reflexes, a tendency to flexion of the body, and monotonous, quiet speech. Syndrome of symmetrical circulatory disorders in the peripheral cortical branches of the middle cerebral artery
(syndrome of bilateral symmetrical softening of the brain) is characterized by fadiolinguomastikatory diplegia with damage to the face, tongue and chewing muscles, phenomena of pseudobulbar paresis with impaired swallowing, phonation, violent laughter and crying.
In case of circulatory disorders in the system of the middle cerebral artery, the following focal dyscirculatory syndromes (syndromes of focal softening) are distinguished.
Precentral dyscirculatory syndrome includes paralysis of the facial muscles, paresis and atrophy of the tongue and masticatory muscles, i.e., cortical suprabulbar syndrome. With a bilateral focus, diplegia of the facial muscles, tongue and masticatory muscles is noted. With left-sided localization, not only paresis of the tongue (dysarthria), motor aphasia, and sometimes alexia are observed.
Central dyscirculatory cortical-subcortical syndrome is manifested by the development of central paralysis without disturbing afferent innervation.
Postcentral dyscirculatory syndrome, caused by damage to the parietal lobe, is characterized by hemianesthesia (disturbances of deep and complex sensitivity predominate), sometimes thalamic pain, impaired coordination and pseudo-athetotic movements. The syndrome resembles thalamic, but differs in the absence of severe hyperpathy, thalamic hyperkinesis. the syndrome is called pseudothalamic. With left-sided localization of the focus, anarthria and apraxia phenomena are noted.
Parietal dyscirculatory syndrome is manifested by ideational apraxia, astereognosis. Temporal dyscirculatory syndrome with a more common focus, temporal-angular syndrome is manifested by homonymous hemianopia, with a focus on the left in combination with sensory aphasia and alexia.
On the electroencephalogram with thrombosis of the middle cerebral artery, interhemispheric asymmetry is detected.
OBLOCKAGE AND STENOSIS OF THE CEREBRAL ARTERIES
Etiology and pathogenesis
Chronic diseases of the aorta and arteries lead to impaired blood flow through the vessels due to obliterating (stenotic) or dilating (aneurysmal) lesions.
The most common causes of obliteration or stenosis of the arteries are:
1) obliterating atherosclerosis;
2) nonspecific aortoarteritis;
3) thromboangiitis obliterans (endarteritis).
Regardless of the cause of vessel obliteration, sometimes more or less pronounced tissue ischemia appears, to eliminate which reconstructive operations are used, taking into account the characteristics of the pathological process. Characteristics of obliterating diseases cerebral vessels below. The blood supply to most of the cerebral hemispheres comes from the basin of the internal carotid argeria. From its pool, blood is supplied to: the internal capsule, subcortical nodes and white subcortical substance, the cortex of the frontal, temporal and parietal lobes. A common cause of circulatory disorders, both transient and persistent, is the occlusion of the carotid artery (thrombosis, stenosis). The carotid artery is affected more often in men than in women. Stenosis and thrombosis as a result of atherosclerosis is usually localized at the bifurcation of the common carotid artery or in the sinus of the internal carotid artery. In rare cases, occlusion of the common or external carotid artery or damage to the carotid arteries on both sides occurs. To the violation cerebral circulation leads pathological tortuosity and kinks of the carotid artery. Severity focal changes in the brain and clinical manifestations in occlusive processes in the carotid arteries depend on the state of the collateral circulation. In case of violation of collateral circulation, small foci of cerebral infarction usually occur, most often in the basin of the middle cerebral artery. With a combined lesion of the extracranial and intracranial sections of the internal carotid artery, the location and size of the cerebral infarction depend on the pathology of the end vessels. With intracranial thrombosis of the internal carotid artery, which is accompanied by dissociation of the arterial circle big brain ascending thrombosis, large foci of infarction develop in the pool of superficial and deep branches of the middle and anterior cerebral arteries, accompanied by massive neurological symptoms and often leading to lethal outcome.
Clinic
Occlusion of cerebral arteries in initial stages proceeds in the form of transient disorders of cerebral circulation. During this period, patients begin to be disturbed by a feeling of weakness, numbness in the limbs, a decrease in visual acuity in one eye, etc. The period of transient ischemic disorders (attacks) can have a different duration. Cerebral circulation disorders with persistent focal syndrome are different. acute form characterized by a sudden apoplexiform onset. The subacute form is formed slowly, within a few hours or 1-2 days. The chronic, or pseudotumorous, form is characterized by a very slow (over several days or even weeks) increase in symptoms. Occlusion of the internal carotid artery is accompanied by the appearance of various neurological symptoms. In 20% of cases, an alternating optic-pyramidal syndrome develops, which is characterized by blindness or decreased vision on the side of the lesion, sometimes in combination with optic nerve atrophy, pyramidal disorders on the opposite side. These violations may appear simultaneously or are volatile in nature. At the same time, either motor or sensory, or visual disturbances appear. The most common symptom in internal carotid artery occlusion is paresis of the opposing limbs, with predominant involvement of the arm (usually of the cortical type). In most cases, monoparesis is more common. With damage to the left carotid artery, aphasia often develops, usually motor. Also there are violations of sensitivity, hemianopsia. Epileptiform seizures are less common.
With intracranial thrombosis of the internal carotid artery, dissociating the arterial circle of the cerebrum, along with hemiplegia and hemihypesthesia, pronounced cerebral symptoms are observed: headache, vomiting, impaired consciousness, psychomotor agitation, secondary stem syndrome as a result of cerebral edema, confusion and compression of the brain stem. When squeezing a healthy carotid artery, dizziness, fainting, and sometimes convulsions in healthy limbs appear. Of particular importance for the diagnosis is angiography.
Diagnostics
In addition to clinical data, additional methods investigations: ultrasound cerebral dopplerography, rheoencephalography, angiography.
Treatment
Carotid artery occlusion is treated conservatively. In some cases it is possible to use surgical methods treatment, which occurs with stenosis as a result of atherosclerosis, as well as the absence or slight severity of persistent neurological symptoms.
Anterior cerebral artery. Superficial branches supply it with blood medial surface frontal and parietal lobes, paracentral lobule, partially orbital surface of the frontal lobe, outer surface of the first frontal gyrus, upper part of the central and superior parietal gyri, most of the corpus callosum (with the exception of its most posterior sections). The central (deep) branches (the largest of them is the Gübner recurrent artery) supply blood to the anterior thigh of the internal capsule, the anterior sections of the head of the caudate nucleus, the shells of the pale ball, partly the hypothalamic region, the ependyma of the anterior horn of the lateral ventricle.
Extensive infarcts covering the entire area of irrigation of the anterior cerebral artery rarely develop. These heart attacks occur as a result of blockage of the trunk of the anterior cerebral artery only after the anterior communicating artery leaves.
Also this pathology occurs with a combined lesion of the vessels involved in the formation of the collateral circulation network through the anterior communicating artery.
Clinic
With extensive cerebral infarctions in the basin of the anterior cerebral artery clinical picture characterized by the appearance of neurological symptoms in the form of spastic paralysis of the proximal upper and distal sections lower limbs on the side opposite the lesion. Often there is a delay or incontinence of urine. Characterized by the presence of a grasping reflex and symptoms of oral automatism. In the case of bilateral cerebral infarction, a violation often develops mental state the patient in the form of aspontaneity, reduced criticism, weakening of memory, etc. Often, in the case of a lesion of the corpus callosum on the left, apraxia of the left hand develops. Sometimes mildly expressed disorders of sensitivity on the paralyzed leg are observed.
In the basin of the anterior cerebral arteries, limited cerebral infarctions most often develop. This fact due to the peculiarities of the network of collateral circulation, as well as the fact that during the atherosclerotic process there is an uneven lesion of the terminal branches of the anterior cerebral artery. In the case of thrombosis or stenosis of the paracentral artery, monoparesis of the foot develops, which can mimic peripheral paresis. Left-sided apraxia occurs in the area supplied by this artery with damage to the coronosal artery and the development of a heart attack in the area supplied by this artery. With damage to the premotor region and pathways from it, the so-called pyramidal cleavage syndrome is observed, when the degree of spasticity significantly dominates the degree of paresis and a rare increase in tendon reflexes is noted while the abdominal ones are preserved; pathological foot reflexes of the flexion type prevail.
Middle cerebral artery - this is the largest of the arteries of the brain, it provides blood to its extensive sections.
There are two branches of the cerebral artery:
1) central (deep) branches that extend from the initial part of the artery trunk and feed most of the subcortical nodes and the internal capsule;
2) cortical branches: the anterior temporal artery, which departs from the initial part of the trunk of the middle cerebral artery and feeds most of the temporal region; ascending branches extending from a common trunk: orbital-frontal, precentral (preroland), central (roland), anterior parietal arteries; posterior parietal, posterior temporal and angular arteries.
Most often, a heart attack develops in the basin of the middle cerebral artery. This is due to the predisposition of the artery to atherosclerotic changes, stenosis, thrombosis, embolism (cardiogenic or arterio-arterial origin). In some cases, cerebral infarction occurs in the presence of an occlusive process in the carotid artery, but in the absence of pathological changes in the middle cerebral artery itself. Most often, cerebral infarction develops as a result of a combined lesion of the internal carotid and middle cerebral arteries.
Clinic
The presence of characteristic symptoms and the degree of its severity in the case of blockage or narrowing of the artery is determined by the localization of the occlusive process, the effectiveness of compensatory mechanisms of collateral circulation, the development of a heart attack and its size. So, due to blockage of the artery trunk to the place of origin of the deep branches, its entire basin is affected (total infarction). If the defect is localized after the place of origin of the deep branches, then the observed pattern of the lesion is more local in nature, covering only the basin of the cortical branches (the cortex and the underlying white matter).
Total infarction in the artery pool covers the posterior frontal gyri, the lower 2/3 of the anterior and posterior central gyri, the opercular region, a significant part of the parietal and temporal region, the insula, the semioval center, the internal capsule (partially anterior femur, knee, anterior posterior femur) , subcortical nodes and part of the thalamus. Most often, circulatory disorders in the basin of the posterior branches of the middle cerebral artery occur with simultaneous damage to the posterior cerebral artery, the vertebrobasilar system.
Clinical Syndrome with a total infarction in the basin of the middle cerebral artery, it consists of contralateral hemiplegia, hemianesthesia and hemianopsia. Left hemispheric infarcts also cause aphasia. mixed type or total, with right hemispheric - anosognosia. If the basin of the posterior cortical branches of the artery does not suffer, then there is no hemianopia, sensory disturbances are less profound, speech is usually impaired by the type of motor aphasia. A heart attack in the pool of deep branches leads to a temporary violation of sensitivity (spastic hemiplegia), with the localization of foci in the left hemisphere, short-term motor aphasia is formed. With an extensive infarction in the basin of the cortical branches, hemiplegia or hemiparesis are noted with a primary lesion of the function of the hand, violations of all types of sensitivity, hemianopsia; with left hemispheric foci, in addition, mixed or total aphasia, impaired counting, writing, reading, apraxia. In right-hemispheric foci in the acute period of a stroke, anosognosia and autotopagnosia often occur.
For a heart attack in the pool of the common trunk of the ascending branches of the artery, the development of hemiplegia or hemiparesis is characteristic with a predominance of dysfunction of the face and hand, hemihypesthesia of the cortical type, with left hemisphere foci - motor aphasia.
With a heart attack in the basin of the posterior branches of the middle cerebral artery, a parietotemporal angular syndrome develops. This syndrome manifests itself the following symptoms: half or lower quadrant hemianopsia, hemihypesthesia with astereognosis. It is also possible to develop afferent paresis of the limbs, which occurs when deep sensitivity is impaired. In left hemispheric lesions, in addition to these symptoms, there are sensory and amnestic aphasia, apraxia, acalculia, agraphia, and digital agnosia. With hemispheric foci, disorders of the body scheme may occur.
Infarcts in the pool of individual branches of the middle cerebral artery occur with more limited symptoms. In the case of a cerebral infarction in the basin of the precentral artery, paralysis of the muscles of the tongue, lower face and masticatory muscles develops. The appearance of motor aphasia indicates the presence of foci in the left hemisphere of the brain. The most severe is bilateral lesion. In this case, a pseudobulbar syndrome develops, which is characterized by a violation of phonation, articulation and the act of swallowing.
With a heart attack in the basin of the central artery, hemiplegia or hemiparesis is observed with a predominance of paresis in the arm (without aphasia). With a heart attack in the basin of the posterior parietal artery, hemihypesthesia or hemianesthesia is noted for all types of sensitivity, sometimes with afferent paresis. This syndrome is called pseudothalamic, but it does not have the pain that is so characteristic of lesions of the visual tubercle. Perhaps the development of heart attacks in the deep parts of the cerebral hemispheres. In this case, the lesions are usually small in size. This type infarcts refers to lacunar infarcts. Their origin is associated with ischemia in the pool of individual striatal arteries, which is often provoked by the presence of concomitant arterial hypertension or atherosclerosis in the patient. In the case of single foci of damage to the brain tissue, the clinic may be erased (mild transient hemiparesis) or absent altogether. Bilateral lacunar infarcts in the lenticular nuclei contribute to the formation of status lacunaris. Lacunar infarctions in the posterior thigh of the internal capsule are usually accompanied by the development of limited symptoms, represented by either monoparesis, hemiparesis, or hemiplegia, or only sensory disturbances. With bilateral small focal lesions of the brain, the so-called lacunar condition develops. The presence of this condition causes the development of syndromes: pseudobulbar and akineticorigid, as well as a decrease in intelligence.
Anterior choroid plexus artery (anterior villous) participates in the blood supply to the back of the thigh (rear two-thirds). In some cases, this artery is involved in the blood supply to the caudate nucleus, the globus pallidus (its internal segments), lower horn(its lateral wall), lateral ventricle, internal capsule (retrolenticular part). The blood supply area of this artery has a highly developed network of anastomoses, which explains the minor neurological symptoms in occlusive lesions of this artery. Most often there is a heart attack of the pale ball (its medial part).
Posterior cerebral artery. Its cortical branches supply blood to the cortex and the underlying white matter of the occipital-parietal region, the posterior and medial-basal regions of the temporal region. The central (deep) branches (thalamo-perforating, thalamo-knee, premamillary) provide blood to a significant part of the optic tubercle, the posterior hypothalamic region, the thickening of the corpus callosum, the optic crown and the subtubercular nucleus (Lewis body); branches also branch off from the artery to the midbrain. As a rule, a heart attack occurs when an artery or its branch is blocked when the main or vertebral artery. Their combined defeat is quite often noted. In connection with numerous anastomoses of the branches of the posterior cerebral artery with other cerebral arteries (middle, anterior, arteries of the choroid plexus), total heart attacks in the basin of this artery are extremely rare. Covering the entire occipital lobe, the third and partly the second temporal lobes, the infarction in the basin of the cortical branches of the posterior cerebral artery also extends to the basal and media-basal gyrus of the temporal lobe (for example, the parahippocampal one).
Clinic
Homonymous hemianopsia or upper square hemianopsia is observed, morphopsia and visual agnosia occur less frequently. Transient amnesia with the subsequent development of alexia, moderately severe sensory aphasia occurs with the development of a heart attack localized in the left hemisphere. In the case of bilateral infarcts in the region of the occipital cortex, the so-called tubular vision develops, associated with the formation of bilateral hemianopsia, and the preservation of macular vision. Perhaps the development of cortical blindness due to insufficiency of anastomoses between the cortical branches of the middle and posterior cerebral arteries in the parts of the occipital cortex responsible for macular vision. The latter is characterized by the preservation of pupillary reactions to light, since the visual pathways from the retina to the brain stem are not damaged. In the case of maintaining the field and visual acuity, or with mild violations of the latter, one or another disorder of higher visual functions. So, with bilateral infarcts at the junction of the parietal and occipital regions, sometimes a syndrome of agnosia on the face (prosopagnosia) occurs, when the patient loses the ability to recognize the faces of relatives and friends while maintaining the ability to recognize surrounding objects. This syndrome of agnosia, in some cases, may be joined by others. pathological changes in the form of a loss of topographic memory, a violation of orientation in space. With an occlusive lesion of the posterior cerebral artery, acquired achromatopsia (color vision impairment) may develop, which usually occurs with a limited bilateral infarction of the occipital lobes of the brain (their lower divisions). The environment appears to the patient at the same time devoid of color (and in severe cases, he perceives everything as black and white),
Clinic
vertebral artery
Etiology and pathogenesis
Clinic
Approximately 75% of cases develop Wallenberg-Zakharchenko, Babinsky-Najotte syndromes and other syndromes of unilateral lesions of the lower parts of the brain stem. The most difficult in terms of prognosis is bilateral thrombosis of the vertebral artery, which develops bulbar paralysis, characterized by a severe disorder of swallowing, phonation, respiration, cardiac activity. In case of blockage of the innominate artery or the initial section subclavian artery subclavian steal syndrome develops, in which there is a violation of blood circulation in the artery. This leads to the occurrence of retrograde blood flow in the vertebral artery on the side of the
blockage due to a drop in pressure in it. With this pathology, part of the blood in the affected vertebral artery is aspirated from the opposite vertebral artery. In this case, the blood enters the subclavian artery and then into the vessels of the arm, "robbing" the brain. All of these pathological changes lead to a restriction of blood flow to the brain stem, the appearance of stem symptoms. If blood enters the vertebral artery from the carotid system, symptoms from the cerebral hemispheres are observed. So, in most cases, the steal syndrome proceeds latently. Expressed clinical symptoms manifests itself when several vessels are affected and compensation processes in the brain are disrupted. If you offer the patient to work hard with his hand with unilateral blockage of the subclavian artery, there is an increase or appearance of stem symptoms, which is explained by an increase in blood flow to this hand.
Arteries of the brain stem . The blood supply to the brain stem is carried out by branches of the main and vertebral arteries, as well as the posterior cerebral artery.
Etiology and pathogenesis
Clinic
Midbrain arteries . The paramedian arteries of the midbrain extending from the main and posterior cerebral arteries are the main ones when the patient loses the ability to recognize the faces of relatives and friends while maintaining the ability to recognize surrounding objects. In some cases, this syndrome of agnosia may be accompanied by other pathological changes in the form of loss of topographic memory, impaired orientation in space. With an occlusive lesion of the posterior cerebral artery, acquired achromatopsia (color vision impairment) may develop, which usually occurs with a limited bilateral infarction of the occipital lobes of the brain (their lower sections). The environment appears to the patient at the same time devoid of color (and in severe cases, he perceives everything as black and white),
With the appearance of foci of infarction in the temporal region (medial-basal regions), Korsakov's syndrome develops, characterized by a violation of working memory and emotional-affective disorders.
For an infarction in the basin of the thalamogeniculate artery, covering the outer part of the ventrolateral nucleus of the thalamic tubercle, the ventral posterolateral nucleus, the lower two-thirds of the caudal nucleus, most of the pillow of the optic tuberosity and the lateral geniculate body, the development of the classic thalamic syndrome (Dejerine-Roussy) is characteristic. This syndrome includes a violation of sensitivity in the form of hemihypesthesia or hemianesthesia, dysesthesia; trophic autonomic disorders; the appearance of hemianopsia, as well as hyperkinesias of an athetic or choreoathetic character, is possible.
Infarction in the basin of the thalamo-perforating artery destroys back hypothalamic region, dorsomedial nucleus of the thalamus opticus, Lewis median nucleus, Lewis body, dentorubrothalamic pathway. The clinical syndrome is severe ataxia and intentional tremor in the contralateral limbs. At times, instead of tremor in the hand, there is hyperkinesis of the choreoathetous type or hemiballismus, tonic setting of the hand (fingers are slightly bent at the metacarpophalangeal joints, the middle and terminal phalanges are unbent, the forearm is bent and pronated, the hand is in the flexion position).
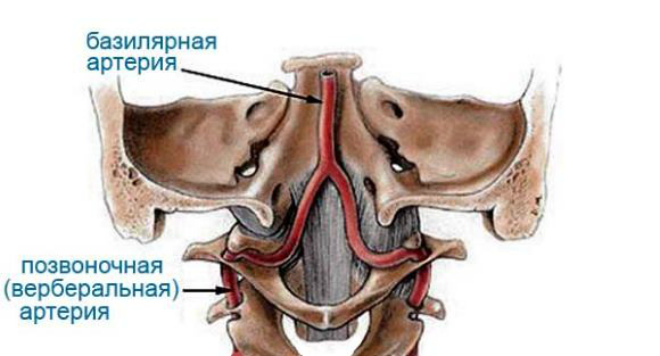
The main artery gives branches to the pons of the brain (pons varolii), the cerebellum and continues with two posterior cerebral arteries.
Clinic
The appearance of repeated circulatory disorders in the vertebrobasilar system, manifested by dysarthria, dizziness attacks, transient paresis and paralysis of the limbs and cranial nerves, is a harbinger of thrombosis of the main artery in 70% of patients.
Acute occlusion (thrombosis) of an artery accompanied by symptoms of a predominant lesion of the brain bridge with a disorder of consciousness up to coma. Within a few hours or 2-5 days, bilateral cranial nerve palsies (II, IV, V, VI, VII), paralysis of the limbs, and impaired muscle tone increase. Bilateral pathological reflexes, symptoms of oral automatism, trismus are often noted. There are narrow (with a pinhead) pupils, vegetative-visceral crises, hyperthermia, disorder of vital functions.
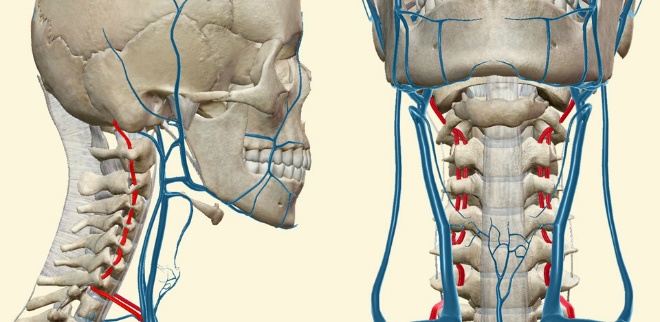
vertebral artery supplies blood to the medulla oblongata cervical region spinal cord(anterior spinal artery), cerebellum.
Etiology and pathogenesis
In most cases, thrombosis, stenosis of atherosclerotic origin, pathological tortuosity of the artery, its kinks, vertebrogenic displacements and compression cause circulatory disorders in the basin of the vertebral artery. In this case, the foci of infarction are localized in the medulla oblongata, cerebellum, in the pool of blood supply to the main and posterior cerebral arteries, since they are also part of the vertebrobasilar system.
Clinic
An occlusive lesion of the extracranial artery is characterized by "spotting" of the lesion of various parts of the basin of the vertebrobasilar system; often there are vestibular disorders (dizziness, nystagmus), disorders of statics and coordination of movements, visual and oculomotor disorders, dysarthria; less pronounced motor and sensory disturbances. In some cases, loss of postural tone is possible, which is accompanied by bouts of sudden falling with the preservation of consciousness. In addition, there may be a memory disorder for current events (such as Korsakoff's syndrome), transient amnesia.
Presence of persistent alternating lesion syndromes medulla oblongata in combination with symptoms of ischemia of the oral parts of the brain stem, occipital and temporal lobes of the brain of a transient nature indicates occlusion of the intercranial vertebral artery.
Approximately 75% of cases develop Wallenberg-Zakharchenko, Babinsky-Najotte syndromes and other syndromes of unilateral lesions of the lower parts of the brain stem. The most severe in terms of prognosis is bilateral thrombosis of the vertebral artery, in which bulbar palsy develops, characterized by a severe disorder of swallowing, phonation, respiration, and cardiac activity. In the case of blockage of the innominate artery or the initial section of the subclavian artery, subclavian steal syndrome develops, in which there is a violation of blood circulation in the artery. This leads to the occurrence of retrograde blood flow in the vertebral artery on the side of the blockage due to a drop in pressure in it. With this pathology, part of the blood in the affected vertebral artery is aspirated from the opposite vertebral artery. In this case, the blood enters the subclavian artery and then into the vessels of the arm, "robbing" the brain. All of these pathological changes lead to a restriction of blood flow to the brain stem, the appearance of stem symptoms. If blood enters the vertebral artery from the carotid system, symptoms from the cerebral hemispheres are observed. So, in most cases, the steal syndrome proceeds latently. Severe clinical symptoms appear when several vessels are affected and compensation processes in the brain are disrupted. If you offer the patient to work hard with his hand with unilateral blockage of the subclavian artery, there is an increase or appearance of stem symptoms, which is explained by an increase in blood flow to this hand.
The pulse in the arteries of this arm is usually absent or very weak; and signs of ischemic muscle damage may also be found. To diagnose subclavian steal syndrome, axillary angiography is performed on the opposite side, while the contrast agent first fills the vertebral artery of the same side, and on subsequent angiograms it is already in the vertebral artery on the side of the lesion.
Arteries of the brain stem. The blood supply to the brain stem is carried out by branches of the main and vertebral arteries, as well as the posterior cerebral artery.
Three groups of branches depart from them:
1) paramedian arteries, feeding mainly the middle parts of the brain stem (at the base);
2) short (enveloping) arteries supplying blood to the lateral sections of the trunk;
3) long circumflex arteries supplying the dorso lateral departments trunk and cerebellum.
Etiology and pathogenesis
With occlusive damage to the arteries of the vertebrobasilar system at various levels, infarcts develop in the brain stem. In some cases, the leading role is played by defeat main vessel, in others - the defeat of the final vessel; their combined defeat often takes place.
Clinic
For damage to the brain stem of an ischemic nature, the appearance of several small foci of infarction, the so-called spotting, is characteristic. This fact explains the presence of a large polymorphism clinical manifestations in each specific case.
Midbrain arteries. The paramedian arteries of the midbrain extending from the main and posterior cerebral arteries mainly pass in the lateral columns of the upper segments of the spinal cord. With the defeat of this part of the spinal cord and the lower parts of the brain stem, the loss of the possibility of automatic breathing develops. The reason is the dissociation of the respiratory center of the medulla oblongata and spinal motor neurons of the respiratory muscles. At the same time, the connection of motor neurons with the cerebral cortex is preserved (Ondine's syndrome).
At the same time, breathing in the state of wakefulness is not disturbed, while in a dream, a severe violation of breathing occurs even before it stops with a fatal outcome.
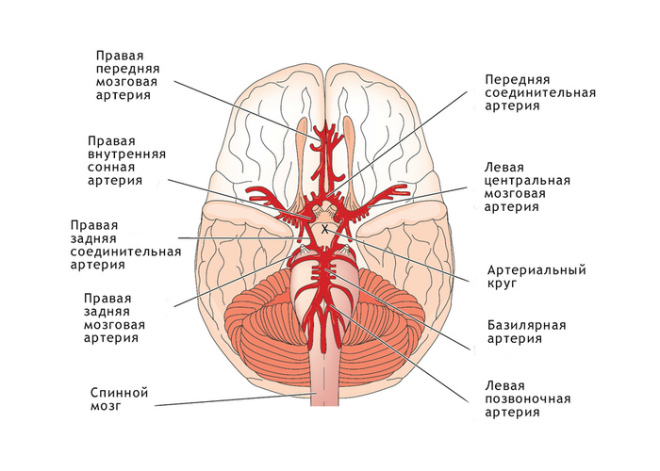
The blood supply to the brain is carried out by paired vertebral and carotid arteries. The carotid arteries account for two-thirds of the transported blood, and the vertebral arterial vessels for the remaining third.
However, the big picture is:
- Vertebrobasilar system:
- carotid pool;
- Circle of Willis.
The human brain needs a sufficient amount of resources for its normal functioning. During the period when the brain is inactive, it consumes about 15% of glucose and oxygen from their total amount, and 15% of all blood in the body passes through it. These needs are primarily necessary to maintain the functions nerve cells, and energy substrate of the brain.
The total blood flow in the human brain is approximately 50 ml of blood per minute per 100 g of brain tissue, and does not change in the process. Between this, the child's blood flow rates are 50% higher than in adults, and in the elderly there is a decrease in these indicators by 20%. Under normal conditions, unchanged blood flow indicators are observed with fluctuations blood pressure 80 to 160 mmHg Art.
It is also worth noting that the overall blood flow is significantly affected by sudden changes in the tension of oxygen and carbon dioxide in the arterial blood, and the stability of the blood flow is maintained by a complex regulatory mechanism.
Blood supply to the brain is carried out by 4 large vessels: two internal carotid and two vertebral arteries. The circulatory system of the brain includes:
- Internal carotid arteries
They are branches of the common carotid arteries, and the left branch branches off from the aortic arch. The left and right carotid arteries are located in the lateral parts of the neck. The characteristic pulsation of their walls can be easily felt through the skin, simply by placing your fingers on the desired point on the neck. Clamping of the carotid arteries leads to impaired blood flow to the brain.
At the level of the upper part of the larynx, the external and internal carotid arteries depart from the common carotid artery. internal artery penetrates the cranial cavity, where it participates in the blood supply to the brain and eyeballs, external - nourishes the organs of the neck, face and skin covering heads.
- Vertebral arteries
These arteries in the brain branch off from the subclavian arteries, pass to the head through a series of holes in the transverse processes of the cervical vertebrae, and subsequently empty into the cranial cavity through the foramen magnum.
Since the vessels that feed the brain branch off from the branches of the aortic arch, therefore, the intensity (velocity) and pressure in them are high, and they also have an oscillatory pulsation. In order to smooth them out, when they flow into the cranial cavity, the internal carotid and vertebral arteries form characteristic bends (siphons).
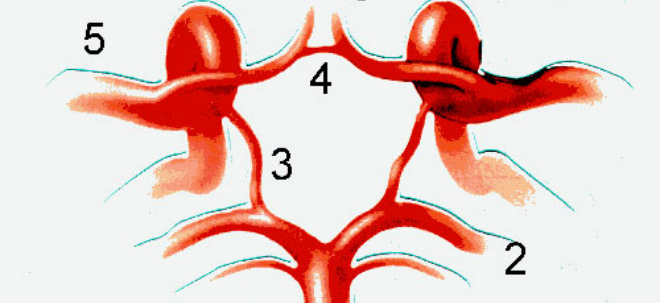
After entering the cranial cavity, the arteries are connected to each other and form the so-called circle of Willis (arterial circle) of the brain. It allows, in case of violation of the blood supply of any of the vessels, to redirect its work to other vessels, which makes it possible to prevent a violation of the blood supply to the brain area. It is worth noting that under normal conditions, blood redistributed through various arteries does not mix in the vessels of the circle of Willis.
3. Cerebral arteries
The anterior and middle cerebral arteries branch off from the internal carotid artery, which in turn feed the internal and external surfaces. hemispheres, as well as deep brain regions.
The posterior cerebral arteries, which feed the occipital lobes of the cerebral hemispheres, the arteries that also feed the brainstem and cerebellum, appear to be branches of the vertebral arteries. From the large cerebral arteries, many thin arteries originate, which subsequently sink into the brain tissue. The diameter of these arteries varies in width and length, therefore they are divided into: short (feeding the cerebral cortex) and long (feeding the white matter).
A high percentage of emerging hemorrhages are patients with existing changes in the walls of the vessels of these particular arteries.
- Blood-brain barrier
Regulation of the transport of substances from blood capillary into the nervous tissue and is called the blood-brain barrier. At normal, various compounds, such as iodine, salt, antibiotics, etc., do not pass from the blood to the brain. Therefore, medical preparations, which have these substances in their composition, have no effect on nervous system person. Conversely, substances such as alcohol, morphine, chloroform easily pass the blood-brain barrier. This is due to the intense effect on the nervous system of these substances.
In order to avoid this barrier, antibiotics and others chemical substances, which are used in the treatment of infectious brain pathologies, are injected directly into the cerebrospinal fluid. For this, a hole is made in lumbar spinal column or in the suboccipital region.
carotid pool
The composition of the carotid basin of the brain includes carotid arterial vessels, which originate from chest cavity. The carotid pool is responsible for the blood supply to most of the head, brain and vision. Upon reaching the thyroid cartilage, the carotid arteries of the brain are divided into internal and external arterial vessels.
When the functions of these blood pathways are impaired, the blood supply to the head becomes unstable and gradually decreases, which ultimately leads to the manifestation of diseases such as ischemia, thrombosis or embolism.
The most common provoking factors of these diseases are atherosclerosis or fibromuscular dysplasia, as well as a number of others. However, as a rule, vascular atherosclerosis is the main pathological factor. With impaired metabolism, cholesterol is gradually deposited on the walls of blood vessels, which subsequently forms atherosclerotic plaques, which leads to the arrest of arterial pathways. Over time, these plaques are destroyed, which can lead to thrombosis.
Vertebrobasilar system
This system is formed from the vertebral arteries and the basilar artery, which is formed as a result of the fusion of the vertebral vessels. The vertebral blood pathways originate in the thoracic cavity and pass through the entire bony canal of the cervical vertebrae, reaching the brain.
The basilar (or formerly the main cerebral artery) is responsible for the blood supply to the posterior regions of the brain. Common diseases are thromboses and aneurysms.
Thrombosis occurs as a result of damage to blood vessels, which can be caused by various causes, from trauma to atherosclerosis. Most negative consequence thrombosis is an embolism that subsequently develops to thromboembolism. The disease is accompanied neurological symptoms, which indicate the defeat of the bridge. Also registered acute disorders brain function and stagnation of blood in the capillaries, which often leads to a stroke.
In the event of an aneurysm of the arteries, this can lead to a possible hemorrhage in the brain and, as a result, the death of its tissues, which ultimately leads to the death of a person.
circle of willis
The circle of Willis includes a network of main arteries of the head and is mainly responsible for the blood supply to the brain tissues. It also consists of paired anterior, posterior and middle cerebral arteries. Depending on the visualization of these vessels, the circle of Willis can be closed (all vessels are visualized) and not closed (when at least one vessel is not visualized).
The key purpose of the circle of Willis is compensatory activity. That is, if there is a lack of incoming blood, the circle of Willis begins to compensate for this deficiency with the help of other vessels, which ensures the smooth operation of the brain.
The appearance of the circle of Willis is not a very frequent occurrence, and is recorded only in 35% of cases. It is often distinguished by its underdevelopment, which is not a pathology, but can lead to a more severe course of certain diseases, since its compensatory functions are not fully realized.
The narrowing of the arteries of the brain, for example, with hypoplasia or with a developing aneurysm, often occurs in the circle of Willis.
Venous outflow
The outflow of blood from the brain is carried out through the system of superficial and cerebral veins, which subsequently flow into the venous sinuses of the solid MO. The superficial cerebral veins (superior and inferior) collect blood from the cerebral cortex and subcortical white matter. In turn, the upper ones fall into the sagittal sinus, the lower ones into the transverse sinus.
Veins located deep in the brain carry out the outflow of blood from the subcortical nuclei, the cerebral ventricles, the internal capsule and subsequently merge into a large cerebral vein. From the venous sinuses there is an outflow of blood through the internal jugular and vertebral veins. Also, the emissary and diploic cranial veins, which connect the sinus with the external cranial veins, provide proper outflow of blood.
From characteristic features cerebral veins are distinguished by the absence of valves in them and a large number of anastomoses. Venous network The brain is characterized by the fact that its wide sinuses provide optimal conditions for the outflow of blood and a closed cranial cavity. Venous pressure in the cranial cavity is almost identical to intracranial pressure. This is a consequence high blood pressure inside the skull venous congestion and a violation of the outflow of blood from the veins with developing hypertension (neoplasms, hematomas).
 The system of venous sinuses includes 21 sinuses (8 paired and 5 unpaired). Their walls are formed by sheets of processes of solid MO. Also on the cut, the sinuses form a wide lumen in the form of a triangle.
The system of venous sinuses includes 21 sinuses (8 paired and 5 unpaired). Their walls are formed by sheets of processes of solid MO. Also on the cut, the sinuses form a wide lumen in the form of a triangle.
The characteristic sinus connection of the cranial base with the veins of the eyes, face and inner ear can be the cause of a developing infection in the sinuses of the dura mater. In addition, when clogging the cavernous or stony sinuses, a pathology of venous outflow through the eye veins is observed, as a result of which facial and periorbital edema occurs.
Blood supply to the spinal cord
The blood supply to the spinal cord is provided by the anterior, two posterior, and radicular-spinal arteries. The artery localized on the anterior surface of the spinal cord originates from two branching vertebral spinal arteries, which subsequently join and form a single trunk. The two posterior spinal arteries, which originate from the vertebrates, run along the dorsal surface of the spinal cord.
The spinal arteries from vertebrates supply blood to only 2 or 3 upper cervical segments, in all other parts of the spinal cord, nutrition is regulated by the radicular-spinal arteries, which in turn receive blood from the vertebral and ascending cervical arteries, and below - from the intercostal and lumbar arteries.
The spinal cord has a highly developed venous system. The veins that drain the anterior and posterior sections of the spinal cord have a "watershed" approximately in the same place as the arteries. The main venous channels, which receive the blood of the veins from the substance of the spinal cord, run in the longitudinal direction, similarly to the arterial trunks. At the top, they connect with the veins of the base of the skull, forming a continuous venous tract. The veins of the spinal cord also have a connection with the venous plexuses of the spine, and through them - with the veins of the body cavities.
Pathologies of the arteries
The human brain for normal functioning spends a huge amount of resources that are supplied in the process of its blood supply. In order to provide these resources in the brain, there are 4 large paired vessels. Also, as we noted earlier, there is a circle of Willis, in which most of the blood tracts are localized.
It is this element that compensates for the lack of incoming blood during the development different nature as well as injuries. If one of the vessels does not supply enough blood, then other vessels compensate for this, to which this deficiency is redistributed.
Therefore, the abilities of the circle of Willis make it possible to compensate for the lack of blood, even with two insufficiently functioning vessels, and a person will not even notice any changes. However, even such a well-coordinated mechanism may not be able to cope with the loads that the patient creates for his body.
The most common symptoms of diseases associated with the pathology of the arteries of the head are:
- Headache;
- Chronic fatigue;
- Vertigo.
With untimely diagnosis, over time, the disease can progress, which results in damage to the brain tissue that occurs with dyscirculatory encephalopathy. This disease is characterized by insufficient blood supply to the brain, in a chronic form.
The main causes of such a pathology are atherosclerosis developing in a patient or arterial hypertension. Since these diseases are quite common, the likelihood of developing dyscirculatory encephalopathy is quite high.
Also, the development of pathology can provoke osteochondrosis. This is due to the fact that with it there is a deformation of the intervertebral discs, which during this pathological process can clamp the vertebral artery of the brain, and also, if the circle of Willis does not cope with its functions, the brain begins to lack the necessary elements for its normal functioning. As a result, the process of death of nerve cells begins, which in turn leads to a number of neurological symptoms.
Dyscirculatory encephalopathy does not decrease with time, but on the contrary, its progressive nature is observed. This creates a high probability of developing a set serious illnesses such as stroke and/or epilepsy. That is why early examinations and treatment are essential in the pathology of the arterial pathways of the brain.
How to improve brain blood supply
It should be noted right away that independent use medicines is not allowed, therefore, almost any restoration of cerebral blood flow must take place with the permission of the attending physician. In order to improve cerebral circulation, the doctor may prescribe the following:
- Drugs that prevent platelets from sticking together;
- Vasodilators;
- Drugs that prevent blood clotting;
- nootropics;
- Psychostimulants.
Also, the patient needs a mandatory adjustment of his diet. Therefore, it is recommended to take products such as:
- oils, for plant-based(pumpkin, olive, linseed);
- Sea and ocean fish products (trout, tuna, salmon);
- Berries (lingonberries, cranberries);
- Bitter chocolate, with a cocoa content of at least 60%;
- Nuts, flax or sunflower seeds;
- Green tea.
Also, in order to improve blood supply and prevent various disorders in the activity of the brain, experts additionally advise, first of all, to avoid physical inactivity. For this great way are physical exercises, which properly activate blood circulation not only in the brain, but throughout the body.
In addition, saunas and baths have a very good effect. Warming up the body improves blood circulation in the brain and body. High efficiency, also has a number of means traditional medicine, for example, periwinkle, propolis and a number of other mixtures are used that have a positive effect on the state of the vessels of the brain.
Video
The middle cerebral artery is the largest of the cerebral arteries; it provides blood to vast areas of the brain. The following branches of the middle cerebral artery are distinguished: a) deep branches (the largest of them are a. putamino-capsulo-caudata, a. lenticulo-striator or a. haemorrhagica), which depart from the initial part of the trunk of the middle cerebral artery and feed a significant part of the basal ganglia and internal capsule; b) cortical-subcortical branches: the anterior temporal artery, which departs from the initial part of the CTBol of the middle cerebral artery and feeds most of the temporal region; ascending branches extending from a common trunk: orbitofrontal, preroland, roland, anterior parietal artery; posterior parietal, posterior temporal and angular arteries.
The basin of the middle cerebral artery is an area in which cerebral infarction develops especially often. This is explained by the fact that the middle cerebral artery is more prone to atherosclerotic changes than other cerebral arteries, leading to a narrowing of its lumen, often complicated by thrombosis. In addition, in the basin of the middle cerebral artery, more often than in the basin of other cerebral arteries, emboli, both cardiogenic and arterio-arterial, are observed. Often, a cerebral infarction occurs as a result of an occlusive process in the carotid artery in the absence of a pronounced pathology of the middle cerebral artery itself.
Clinical syndromes that develop with blockage and narrowing of the middle cerebral artery are associated with the size of the infarction and its localization, which in turn depends on the level of the occlusive process and the efficiency of collateral circulation.
If the trunk of the middle cerebral artery is damaged before the deep branches diverge, its entire basin may suffer (total infarction), if the trunk of the middle cerebral artery is damaged after the deep branches diverge, only the pool of cortical-subcortical branches suffers (extensive cortical-subcortical infarction).
A total infarction in the basin of the middle cerebral artery covers the posterior sections of the 1st, 2nd, 3rd frontal gyrus, the lower two-thirds of the precentral and postcentral gyrus, the opercular region, a significant part of the parietal and temporal region, the insula, the semioval center, the internal capsule (partially anterior femur , knee, anterior sections of the posterior thigh), subcortical nodes and part of the thalamus. The basin of the posterior branches of the middle cerebral artery usually suffers only with concomitant damage to the vertebrobasilar system or the posterior cerebral artery.
The clinical syndrome in total infarction in the basin of the middle cerebral artery consists of contralateral hemiplegia, hemianesthesia and hemianopsia. With left-hemispheric infarcts, aphasia occurs (mixed or total), with right-hemispheric infarcts - anosognosia. If the basin of the posterior cortical-subcortical branches of the middle cerebral artery does not suffer, then hemianopsia is absent, sensitivity disturbances are less profound, speech is usually impaired by the type of motor aphasia. With a heart attack in the pool of deep branches, spastic hemiplegia is observed, inconsistently - a violation of sensitivity, with foci in the left hemisphere - short-term motor aphasia. With an extensive cortical-subcortical infarction in the basin of the middle cerebral artery, hemiplegia or hemiparesis is noted with a primary lesion of the function of the hand, a violation of all types of sensitivity, hemianopsia, with left hemispheric foci - mixed or total aphasia, impaired counting, writing, reading, apraxia. In right-hemispheric foci in the acute period of a stroke, anosognosia and autotopagnosia often occur.
A heart attack in the basin of the common trunk of the ascending branches of the middle cerebral artery is accompanied by hemiplegia or hemiparesis with a predominant dysfunction of the hand, cortical-type hemihypesthesia, and motor aphasia in left hemisphere foci.
The infarction in the basin of the posterior branches of the middle cerebral artery is manifested by the so-called parietal-temporal-angular syndrome, including hemianopsia (half or lower quadrant) and hemihypesthesia with astereognosis; in connection with a violation of sensitivity, especially deep, the so-called afferent paresis of the limbs may occur. In left hemispheric lesions, in addition to these symptoms, there are sensory and amnestic aphasia, an-raxia, acalculia, agraphia and digital agnosia. With right-hemispheric foci, disorders of the body scheme may occur.
Infarcts in the pool of individual branches of the middle cerebral artery occur with more limited symptoms. With a heart attack in the basin of the preroland artery, paralysis is observed mainly in the lower part of the face, tongue and chewing muscles; with left-sided foci, motor aphasia occurs. With bilateral foci in this area, a pseudobulbar syndrome develops with impaired articulation, swallowing and phonation.
With a heart attack in the basin of the Roland artery, hemiplegia or hemiparesis is observed with a predominance of paresis in the arm (without aphasia). With a heart attack in the basin of the posterior parietal artery, hemihypesthesia or hemianesthesia is noted for all types of sensitivity, sometimes with "afferent" paresis. This syndrome is called "pseudo-thalamic", but with it there are no pains, so characteristic of the defeat of the thalamic thalamus.
The anterior villous artery takes part in the blood supply to the posterior two-thirds of the posterior femur, and sometimes the retrolenticular part of the internal capsule, caudate nucleus, internal segments of the globus pallidus, and the lateral wall of the lower horn of the lateral ventricle. The clinical syndrome observed during a heart attack in the basin of this artery includes hemiplegia, hemianesthesia, sometimes hemianopsia, and vasomotor disorders in the area of paralyzed limbs. Aphasia (unlike infarction in the basin of the middle cerebral artery) is absent.
Posterior cerebral artery. Its cortical-subcortical branches supply blood to the cortex and the underlying white matter of the occipital-parietal region, the posterior and mediobasal regions of the temporal region. crown and Lewis body; branches also branch off from the artery to the midbrain.
Heart attacks in the basin of the posterior cerebral artery occur both due to blockage of the artery itself or its branches, and Ifr due to damage to the main or vertebral arteries. Quite often their combined defeat takes place.
The branches of the posterior cerebral artery anastomose with other arteries (middle, anterior, villous, with the branches of the main one): in connection with this, total heart attacks in the basin of the posterior cerebral artery almost never occur.
A heart attack in the basin of the cortical-subcortical branches of the posterior cerebral artery can capture the entire occipital lobe, the third and partly the second temporal gyrus, the basal and mediobasal gyrus of the temporal lobe (in particular, the hippocampal gyrus). Clinically, there is homonymous hemianopsia or upper quadrant hemianopsia; the phenomena of metamorphopsia and visual agnosia occur less frequently. With left-hemispheric infarctions, alexia and unsharply expressed sensory aphasia can be observed.
When the infarction spreads to the mediobasal parts of the temporal region, pronounced memory disorders such as Korsakoff's syndrome occur with a predominant impairment of short-term (operational) memory and emotional-affective disorders.
Pool infarction a. thaiamogenicuiata covers the outer part of the ventrolateral nucleus of the thalamus, the ventral posterolateral nucleus, the lower two-thirds of the caudal nucleus, most of the thalamus, and the lateral geniculate body. With the defeat of this area, the classic thalamic Dejerine-Roussy syndrome occurs, including hemihypesthesia or hemianesthesia, as well as hyperpathy and dysesthesia, thalamic pain in the opposite half of the body, transient contralateral hemiparesis; hemianopsia, hyperkinesis of an athetotic or choreoathetotic nature, hemiataxia, trophic and vegetative disorders are observed inconsistently.
Pool infarction a. thalamoperforata destroying the posterior part of the hypothalamic region, the dorso-medial nucleus of the thalamus opticus, the median nucleus, the Lewis body, the dentato-rubrothalamic pathway.
The clinical syndrome is characterized by severe ataxia and intentional tremor in the contralateral limbs. Sometimes, instead of a tremor in the hand, there is hyperkinesis of the choreoathetous type or hemiballismus. A peculiar tonic setting of the hand can also be observed - the "thalamic" hand: the forearm is bent and pronated, the hand is also in the flexion position, the fingers are slightly bent at the metacarpophalangeal joints, the middle and terminal phalanges are unbent.
Middle cerebral artery and other articles on neurology.
The blood supply to the brain is carried out by the vertebral and internal carotid arteries. From the latter in the cranial cavity departs ophthalmic artery. The internal carotid artery itself divides into the anterior and middle cerebral arteries. The vertebral arteries join together to form the basilar artery. It, in turn, is divided into two posterior cerebral arteries. The vertebral-basilar arterial system is connected to the internal carotid arteries, resulting in the formation of an arterial circle of the cerebrum, which acts as a cerebral anastomosis. The outflow of blood from the cerebral cortex is carried out through the veins that form the venous anastomotic network. The outflow of blood occurs in the venous sinuses of the solid meninges.
Chronic diseases of the aorta and arteries lead to impaired blood flow through the vessels due to obliterating (stenotic) or dilating (aneurysmal) lesions. The most common causes of obliteration or stenosis of the arteries are:
1) obliterating atherosclerosis;
2) nonspecific aortoarteritis;
3) thromboangiitis obliterans (endarteritis). Regardless of the cause of vessel obliteration, sometimes more or less pronounced tissue ischemia appears, to eliminate which reconstructive operations are used, taking into account the characteristics of the pathological process. The characteristics of obliterating diseases of the cerebral vessels are given below.
1. Internal carotid artery
It supplies blood to most of the hemispheres - the cortex of the frontal, parietal, temporal regions, subcortical white matter, subcortical nodes, the internal capsule. Occlusive lesion of the carotid artery (thrombosis, stenosis) - common cause transient and persistent circulatory disorders; In men, pathology of the carotid artery is more common than in women.
Atherosclerotic stenosis and thrombosis are more common in the bifurcation of the common carotid artery or in the sinus of the internal carotid artery. Less common is an occlusive lesion of the common or external carotid artery or carotid arteries on both sides. Pathological tortuosity and kinks of the carotid artery can also lead to impaired cerebral circulation.
The severity of focal changes in the brain and clinical manifestations in occlusive processes in the carotid arteries depend mainly on the state of collateral circulation.
With insufficiency of collateral circulation, small foci of cerebral infarction usually occur in areas of adjacent blood supply in the cortical-subcortical regions of the hemisphere, mainly in the basin of the middle cerebral artery. If the occlusive process in the extracranial part of the internal carotid artery is combined with damage to the intracranial arteries, then the size of the infarction and its topic largely depend on the pathology of the end vessels.
With intracranial thrombosis of the internal carotid artery, accompanied by dissociation of the cerebral arterial circle by ascending thrombosis, extensive foci of infarction develop in the basin of the superficial and deep branches of the middle and anterior cerebral arteries, accompanied by massive neurological symptoms and often leading to death. An occlusive lesion in its initial period proceeds in the form of transient cerebrovascular accidents: patients experience short-term numbness and weakness in the limbs, sometimes aphasic disorders, and some have decreased vision in one eye or other symptoms. The period of transient ischemic disorders (attacks) can have a different duration.
Cerebral circulation disorders with persistent focal syndrome proceed differently. The acute form is characterized by a sudden apoplectiform onset. The subacute form develops slowly, over several hours or 1–2 days. The chronic, or pseudotumorous, form is characterized by a very slow (over a number of days or even weeks) increase in symptoms.
Neurological symptoms in occlusive lesions of the internal carotid artery are diverse. Approximately 20% of cases have an alternating optic-pyramidal syndrome: blindness or decreased vision, sometimes with atrophy of the optic nerve on the side of the affected artery and pyramidal disorders on the opposite side.
These disorders can occur simultaneously or sometimes dissociate: either visual, motor or sensory disorders appear. Most common symptom- paresis of opposite limbs, usually of the cortical type with a more severe lesion of the hand, sometimes only monoparesis.
With damage to the left carotid artery, aphasia often develops, usually motor. There may also be sensory disturbances, hemianopsia. Occasionally, epileptiform seizures are noted.
With intracranial thrombosis of the internal carotid artery, which disconnects the arterial circle of the large brain, along with hemiplegia and hemihypesthesia, pronounced cerebral symptoms are observed: headache, vomiting, impaired consciousness, psychomotor agitation, secondary stem syndrome as a result of cerebral edema, displacement and compression of the brain stem. Compression of a healthy carotid artery causes dizziness, sometimes fainting, convulsions in healthy limbs. Angiography is of great importance for diagnosis.
With occlusive lesions of the carotid artery, in addition to conservative treatment, can be applied surgical intervention, which is most appropriate for atherosclerotic stenosis and in the absence or low severity of persistent neurological symptoms.
2. Anterior cerebral artery
Its superficial branches supply blood to the medial surface of the frontal and parietal lobes, the paracentral lobule, partly the orbital surface of the frontal lobe, the outer surface of the first frontal gyrus, the upper part of the central and superior parietal gyrus, most of the corpus callosum (with the exception of its most posterior parts). The central (deep) branches (the largest of them is the recurrent artery of Gubner) supply blood to the anterior thigh of the internal capsule, the anterior sections of the head of the caudate nucleus, the shell of the pale ball, partly the hypothalamic region, the ependyma of the anterior horn of the lateral ventricle.
Extensive infarcts covering the entire area of irrigation of the anterior cerebral artery rarely develop. They can occur when the trunk of the anterior cerebral artery is blocked after the anterior communicating artery leaves it, as well as with combined vascular lesions that prevent the development of compensating collateral circulation through the anterior communicating artery.
The clinical picture with extensive infarcts in the basin of the anterior cerebral artery is characterized by spastic paralysis of the limbs of the opposite side - the proximal arm and distal leg. Often there is a delay (or incontinence) of urine. Characterized by the presence of a grasping reflex and symptoms of oral automatism. With bilateral foci, a mental disorder is often noted (aspontaneity, reduced criticism, weakening of memory, etc.). Often there is apraxia of the left hand (with left-sided foci) as a result of damage to the corpus callosum. Sometimes mildly expressed disorders of sensitivity on the paralyzed leg are observed.
More often in the basin of the anterior cerebral arteries, limited infarctions develop due to the peculiarities of the collateral circulation and uneven damage to the terminal branches of the anterior cerebral artery by the atherosclerotic process.
With a lesion in the supply zone of the paracentral artery, monoparesis of the foot usually develops, simulating peripheral paresis; when the area supplied by the coronosal artery is affected, left-sided apraxia occurs.
With damage to the premotor region and pathways from it, the so-called pyramidal splitting syndrome can be observed, when the degree of spasticity significantly prevails over the degree of paresis and there is a sharp increase in tendon reflexes while the abdominal ones are preserved; pathological foot reflexes of the flexion type prevail.
3. Middle cerebral artery
The largest of the arteries of the brain - provides blood to its vast sections. The following branches of the cerebral artery are distinguished:
1) central (deep) branches that extend from the initial part of the artery trunk and feed a significant part of the subcortical nodes and the internal capsule;
2) cortical branches: the anterior temporal artery, which departs from the initial part of the trunk of the middle cerebral artery and feeds most of the temporal region; ascending branches extending from a common trunk: orbital-frontal, precentral (preroland), central (roland), anterior parietal arteries; posterior parietal, posterior temporal and angular arteries. The basin of the middle cerebral artery is an area in which a heart attack develops especially often due to the fact that this artery is more than other arteries of the brain, is prone to atherosclerotic changes, stenosis, thrombosis, and embolisms, both cardiogenic and arterioarterial.
Sometimes a cerebral infarction occurs as a result of an occlusive process in the carotid artery in the absence of a pronounced pathology of the middle cerebral artery itself, but more often there is a combined lesion of the internal carotid and middle cerebral arteries.
The clinical picture of blockage and narrowing of the artery depends on the size of the infarction and its localization, which, in turn, is associated with the level of the occlusive process and the efficiency of collateral circulation.
If the artery trunk is damaged before the deep branches depart, its entire basin may suffer (total infarction), if the arterial trunk is damaged after the deep branches depart, only the pool of cortical branches (cortex and underlying white matter) suffers. Total infarction in the artery pool covers the posterior frontal gyri, the lower 2/3 of the anterior and posterior central gyri, the opercular region, a significant part of the parietal and temporal region, the insula, the semioval center, the internal capsule (partially anterior femur, knee, anterior posterior femur) , subcortical nodes and part of the thalamus. The basin of the posterior branches of the artery usually suffers only with concomitant damage to the vertebrozasiller system or the posterior cerebral artery.
The clinical syndrome in total infarction in the basin of the middle cerebral artery consists of contralateral hemiplegia, hemianesthesia and hemianopsia.
With left hemispheric infarcts, at the same time, mixed-type aphasia or total aphasia occurs, with right hemisphere infarcts - anosognosia. If the basin of the posterior cortical branches of the artery does not suffer, then there is no hemianopia, sensory disturbances are less profound, speech is usually impaired by the type of motor aphasia.
With a heart attack in the pool of deep branches, spastic hemiplegia is observed, inconsistently - a violation of sensitivity, with foci in the left hemisphere - short-term motor aphasia.
With an extensive infarction in the basin of the cortical branches, hemiplegia or hemiparesis is noted with a predominant lesion of the function of the hand, violations of all types of sensitivity, hemianopsia, with left hemispheric foci, in addition, aphasia of a mixed type or total, impaired counting, writing, reading, apraxia. In right-hemispheric foci in the acute period of a stroke, anosognosia and autotopagnosia often occur.
Infarction in the basin of the common trunk of the ascending branches of the artery is accompanied by hemiplegia or hemiparesis with a predominant dysfunction of the face and hands (brachiofacial type of paresis), hemihypesthesia of the cortical type, with left hemisphere foci - motor aphasia.
Infarction in the basin of the posterior branches is manifested by the so-called parietal-temporal angular syndrome: half or lower square hemianopsia) and hemihypesthesia with astereognosis; with a severe violation of sensitivity, especially deep, the so-called afferent paresis of the extremities may develop. In left hemispheric lesions, in addition to these symptoms, there are sensory and amnestic aphasia, apraxia, acalculia, agraphia, and digital agnosia. With hemispheric foci, disorders of the body scheme may occur.
Infarcts in the pool of individual branches of the middle cerebral artery occur with more limited symptoms.
With a heart attack in the basin of the precentral artery, paralysis is observed mainly in the lower part of the face, tongue and chewing muscles, with left-sided foci, motor aphasia occurs.
With bilateral foci in this area, a pseudo-bulbar syndrome develops with impaired articulation, swallowing and phonation.
With a heart attack in the basin of the central artery, hemiplegia or hemiparesis is observed with a predominance of paresis in the arm (without aphasia). With a heart attack in the basin of the posterior parietal artery, hemihypesthesia or hemianesthesia is noted for all types of sensitivity, sometimes with afferent paresis. This syndrome is called pseudothalamic, but it does not have the pain that is so characteristic of lesions of the visual tubercle.
Heart attacks that occur in the deep parts of the hemispheres are often small in size, associated with ischemia in the pool of individual striatal branches and often refer to the so-called lacunar heart attacks; in most cases, they occur in patients arterial hypertension but may also occur in patients with atherosclerosis.
Solitary lacunar infarcts in this area may clinically go unnoticed or be accompanied by very mild transient hemiparesis.
Bilateral lacunar infarcts in the lenticular nuclei contribute to the formation of status lacunaris. Lacunar infarctions in the posterior thigh of the internal capsule are usually accompanied by the development of limited symptoms, represented by either monoparesis, hemiparesis or hemiplegia, or only sensory disturbances. Bilateral small focal brain damage (lacunar condition) can cause the development of pseudobulbar syndrome, akineticorigid syndrome, and decreased intelligence.
4. Anterior artery of the choroid plexus
The anterior villous artery takes part in the blood supply to the posterior 2/3 of the posterior femur, and sometimes to the retrolenticular part of the internal capsule, caudate nucleus, internal segments of the globus pallidus, the lateral wall of the lower horn, and the lateral ventricle. With occlusion of this artery, the neurological deficit is insignificant, since the area irrigated by it has a rich network of anastomoses; more regularly there is a heart attack of the medial part of the pale ball.
5. Posterior cerebral artery
Its cortical branches supply blood to the cortex and the underlying white matter of the occipital-parietal region, the posterior and medial-basal regions of the temporal region.
Central (deep) branches (thalamo-perforating, thalamo-knee, premamillary provide blood to a significant part of the optic tubercle, posterior hypothalamic region, thickening of the corpus callosum, optic crown and hypotuberous nucleus (Lewis) body); branches also branch off from the artery to the midbrain.
Infarctions in the arterial pool occur due to blockage of the artery or its branches, as well as due to damage to the main or vertebral arteries.
Their combined defeat is often noted. The branches of the posterior cerebral artery anastomose with other arteries - the middle, anterior, arteries of the choroid plexus, branches of the main artery; in this regard, total cerebral infarcts in the basin of the posterior cerebral artery almost never occur.
A heart attack in the basin of the cortical branches of the posterior cerebral artery can capture the entire occipital lobe, the third and partly the second temporal gyrus, the basal and medial-basal gyrus of the temporal lobe (in particular, the parahippocampal gyrus).
clinical picture. Homonymous hemianopsia or upper square hemianopsia is observed, morphopsia and visual agnosia occur less frequently. With left-hemispheric infarctions, alexia and unsharply expressed sensory aphasia can be observed. Sometimes they are preceded by transient amnesias.
Bilateral infarcts in the occipital cortex may be accompanied by "tubular" vision due to bilateral hemianopia with the preservation of macular vision. If the anastomoses between the cortical branches of the middle and posterior cerebral arteries in the parts of the occipital cortex responsible for macular vision are insufficient, then “cortical” blindness occurs. The latter is characterized by the preservation of the reaction of the pupils to light, since the visual pathways from the retina to the brain stem are not damaged.
If the visual fields and visual acuity in cerebral infarcts in the basin of the posterior cerebral arteries are not grossly disturbed, then certain violations of higher visual functions may be detected. So, with bilateral infarcts at the junction of the parietal and occipital regions, sometimes a syndrome of agnosia on the face (prosopagnosia) occurs, when the patient loses the ability to recognize the faces of relatives and friends while maintaining the ability to recognize surrounding objects.
The same syndrome with the same localization may be accompanied by a violation of orientation in space, loss of topographic memory. With limited bilateral infarcts in the lower parts of the occipital lobes, sometimes there is a violation of color vision (acquired achromatopsia). The environment appears to the patient at the same time devoid of color, and in severe cases, he perceives everything as black and white.
When the infarction spreads to the medial-basal parts of the temporal region, pronounced memory disorders such as Korsakoff's syndrome occur with a predominant violation of short-term (operational) memory, emotional-affective disorders.
The infarction in the basin of the thalamo-geniculate artery covers the outer part of the ventrolateral nucleus of the thalamic tubercle, the ventral posterolateral nucleus, the lower 2/3 of the caudal nucleus, most of the pillow of the optic tuberosity and the lateral geniculate body.
With the defeat of this area, the classic thalamic Dejerine-Roussy syndrome occurs, including hemihypesthesia or hemianesthesia, as well as hyperpathy and dysesthesia, thalamic pain in the opposite half of the body, transient contralateral hemiparesis; hemianopsia, hyperkinesis of an athetotic or choreoathetotic nature, hemiataxia, trophic and vegetative disorders are observed inconsistently.
The infarction in the pool of the thalamo-perforating artery destroys the posterior part of the hypothalamic region, the dorsomedial nucleus of the thalamus opticus, the median nucleus of Lewis, the body of Lewis, and the dentorubrothalamic pathway. The clinical syndrome is characterized by severe ataxia and intentional tremor in the contralateral limbs. Sometimes, instead of a tremor in the hand, there is hyperkinesis of the choreoathetous type or hemiballismus.
A peculiar tonic setting of the hand can also be observed - the thalamic hand: the forearm is bent and pronated, the hand is also in the flexion position, the fingers are slightly bent at the metacarpophalangeal joints, the middle and terminal phalanges are unbent.
6. Main artery
It gives branches to the pons of the brain (pons), the cerebellum and continues with two posterior cerebral arteries. In 70% of patients, complete blockage (thrombosis) of the artery is preceded by multiple transient circulatory disorders in the vertebrasillary system - dizziness attacks, dysarthria, transient paresis and paralysis of the limbs, cranial nerves and other symptoms.
Acute occlusion (thrombosis) of the artery is accompanied by symptoms of a predominant lesion of the brain bridge with a disorder of consciousness up to coma. Within a few hours or 2–5 days, bilateral cranial nerve palsies (II, IV, V, VI, VII), paralysis of the limbs, and impaired muscle tone increase. Bilateral pathological reflexes, symptoms of oral automatism, trismus are often noted. There are narrow (with a pinhead) pupils, vegetative-visceral crises, hyperthermia, disorder of vital functions.
7. Vertebral artery
It supplies blood to the medulla oblongata, partly to the cervical spinal cord (anterior spinal artery), and the cerebellum. Atherosclerotic stenosis, thrombosis, vertebrogenic displacement and compression, pathological tortuosity and kinks of the artery are often the causes of cerebral circulation disorders in the basin of the vertebral artery.
Foci of infarction during arterial occlusion can develop not only in the medulla oblongata and cerebellum, but also at a distance - in the blood supply pool of the main and posterior cerebral arteries, since they are parts of a single vertebrobasilar system.
clinical picture. An occlusive lesion of the extracranial artery is characterized by "spotting" of the lesion of various parts of the pool of the vertebrasil system; often there are vestibular disorders (dizziness, nystagmus), disorders of statics and coordination of movements, visual and oculomotor disorders, dysarthria; less pronounced motor and sensory disturbances. Some patients have attacks of a sudden fall due to the loss of postural tone, while consciousness does not turn off. Quite often there are memory disorders, especially for current events, such as Korsakoff's syndrome, and transient amnesia.
Blockage of the intracranial artery is characterized by a combination of persistent alternating syndromes of lesions of the medulla oblongata with symptoms of transient ischemia of the oral parts of the brain stem, occipital and temporal lobes. Approximately 75% of cases develop Wallenberg-Zakharchenko, Babinski-Najotte syndromes and other syndromes of unilateral lesions of the lower parts of the brain stem. With bilateral thrombosis of the vertebral artery, there is a severe disorder of swallowing, phonation, respiratory and cardiac disorders (bulbar palsy).
Sometimes discirculation in the artery occurs due to the so-called subclavian steal syndrome, caused by blockage of the innominate artery or the initial subclavian. Under these conditions, the pressure in the vertebral artery on the side of the blockage drops, a retrograde blood flow occurs in it, sucking part of the blood from the opposite vertebral artery, “robbing” the brain, while the blood enters the subclavian artery and further into the vessels of the arm.
As a result, blood flow to the brain stem is limited, and table symptoms may appear, and sometimes symptoms from the cerebral hemispheres, if blood also enters the vertebral artery on the side of the lesion from the carotid system. In many cases, subclavian steal syndrome proceeds latently: clinical symptoms appear only when several vessels supplying the brain are affected, which limits the processes of compensation. The appearance or intensification of stem symptoms can be caused by inviting the patient to work hard with his hand in case of homolateral blockage of the subclavian artery, which is accompanied by an increase in blood flow to it. The pulse on the arteries of this arm is usually absent or sharply weakened, sometimes there are signs of ischemic muscle damage. To diagnose subclavian steal syndrome, axillary angiography is performed on the opposite side, while the contrast agent first fills the vertebral artery of the same side, and on subsequent angiograms it is already in the vertebral artery on the side of the lesion.
8. Arteries of the brain stem
The blood supply to the brain stem is carried out by branches of the main and vertebral arteries, as well as the posterior cerebral artery. Three groups of branches depart from them: paramedian arteries, feeding mainly the middle parts of the brain stem at the base); short (enveloping) arteries supplying blood to the lateral sections of the trunk, and long envelope arteries supplying the dorsolateral sections of the trunk and cerebellum.
Infarctions in the region of the brain stem are the result of damage to the arteries of the vertebrasil system at various levels. In some cases, the leading role is played by the lesion of the main vessel, in others - the lesion of the final vessel, often their combined lesion takes place.
clinical picture. For ischemic lesions the brain stem is characterized by the well-known "spotting", the dispersion of several, usually small, foci of infarction. Hence the large polymorphism of clinical manifestations in different cases.
9. Arteries of the midbrain
The paramedian arteries of the midbrain depart from the posterior cerebral and basilar arteries and feed mainly on the middle and medial parts of the legs of the brain.
clinical picture. With a heart attack in the pool of these arteries, the so-called lower red nucleus syndrome most often develops - paralysis of the oculomotor nerve on the side of the focus, ataxia and intentional trembling in the contralateral limbs; sometimes there is also choreiform hyperkinesia. With a heart attack that captures the base of the legs of the brain, Weber's syndrome develops. The defeat of the posterior longitudinal beam causes paralysis or paresis of the gaze, which is sometimes combined with nystagmus.
Short circumflex arteries of the midbrain supply blood to the lateral sections of the legs of the brain. It is believed that heart attacks in the area of their blood supply are manifested by paresis of opposite limbs and hemihypesthesia. The long circumflex arteries of the midbrain are branches of the superior cerebellar artery (branches of the basilar artery) and the quadrigeminal artery (branches of the posterior cerebral artery); they provide blood to the superior cerebellar peduncle, spinothalamic bundle, partially lateral and medial loops, central tegmental bundle, mesencephalic root trigeminal nerve, mesh substance, partly quadrigemina.
When the basin of the superior cerebellar artery is affected, choreiform and athetoid hyperkinesias are observed on the side of the focus, a violation of lateral and temperature sensitivity on the opposite side, and sometimes myoclonus of the soft palate. With a heart attack in the pool of the quadrigeminal artery, symptoms of damage to the nuclei of the oculomotor nerve are observed, up to complete ophthalmoplegia, as well as paresis and paralysis of the gaze. Often cerebellar symptoms are also found. With extensive, especially bilateral, infarcts in the midbrain area affecting the nuclei reticular formation, disturbances of consciousness and sleep function are very often noted; sometimes there is peduncular hallucinosis in the form of peculiar visual hallucinations hypnagogic type, i.e., appearing during the period of falling asleep.
10. Arteries of the brain bridge
The paramedian arteries arise from the basilar artery and supply blood mainly to the base of the pons: the pyramidal tracts, the gray nuclei of the pons, the pons' own fibers, and part of the medial loop. In the region of the tire, the nucleus of the abducens nerve sometimes suffers.
Infarction in this area is characterized by contralateral hemiplegia, central paralysis of the facial and hypoglossal nerves (medial pontine infarction). Muscle tone in paralyzed limbs in the initial period after a stroke is usually reduced, defensive reflexes absent or weakly expressed. When the infarction is localized in the lower part of the bridge, paresis of the gaze of the bridge type is noted (the eyes look at the paralyzed limbs) or paralysis of the abducens nerve on the side of the focus. Sometimes this is accompanied by peripheral paralysis facial nerve on the same side.
Bilateral infarction in the basin of the paramedian pontine arteries leads to tetraplegia or tetraparesis, pseudobulbar and cerebellar syndromes. With limited infarcts at the base of the bridge, mild hemiparesis, sometimes monoparesis of the limbs, sometimes only pseudobulbar syndromes, may develop. This is due to the fact that the pyramidal and corticobulbar pathways are located there in the form of separate bundles among their own cells and fibers of the brain bridge.
Short envelope branches depart from the main artery and supply blood to the lateral sections of the brain, sometimes the spinothalamic tract, as well as the lateral parts of the medial loop and pyramidal tract. Infarction in the pool of these branches leads to the development of lateral pontine syndrome. With a heart attack in the middle third of the lateral part of the bridge, the nucleus of the trigeminal nerve can be affected, with a focus in the lower third of the lateral part of the bridge, the nucleus of the facial nerve.
Clinically, the most frequently observed homolateral cerebellar syndrome, combined with a violation of sensitivity, and sometimes pyramidal signs on the opposite side; Horner's syndrome may be noted on the side of the focus.
With lesions in the middle and lower third of the lateral part of the bridge, due to the damage to the sensitivity of the nucleus, the gelatinous substance of the trigeminal nerve and the spinothalamic bundle, there is a disorder of pain and temperature sensitivity of the skin of the face on the side of the focus and a disorder of these types of sensitivity on the opposite side of the trunk and extremities, i.e. Alternating hemihypesthesia or hemianesthesia may occur. With lesions in the lower third of the lateral part of the bridge, along with the main syndrome, peripheral paralysis of the facial nerve on the side of the focus may occur.
The long lateral arteries are branches of the three cerebellar arteries: superior, inferior, and anteroinferior.
The infarction of the oral parts of the tegmentum of the brain bridge in the area of blood supply to the superior cerebellar artery covers the superior cerebellar peduncle, the spinothalamic bundle, the central pathway of the tegmentum, and partly the posterior longitudinal bundle. Clinically, there is a disorder of pain and temperature sensitivity on the side opposite to the focus, cerebellar disorders on the homolateral side, paresis of the gaze of the bridge type, sometimes nystagmus when looking towards the focus. This may be accompanied by hyperkinesis of a choreiform or athetoid nature and Horner's syndrome on the side of the focus, sometimes myoclonic syndrome.
With concomitant discirculation in the short circumflex arteries of the pons, the nucleus of the trigeminal nerve may suffer, sometimes there is a syndrome of alternating hemihypesthesia or hemianesthesia.
Infarction in the caudal part of the pontine tegmentum, which is supplied by the anteroinferior artery of the cerebellum and short circumflex arteries, is accompanied by mild homolateral cerebellar symptoms, dissociated sensitivity disorder on the opposite half of the body, sometimes peripheral paralysis of the facial nerve on the side of the focus.
With bilateral infarcts in the area of the bridge, pseudobulbar syndrome is clearly expressed. With extensive infarcts in the region of the pontine tire, occurring with damage to the activating sections of the reticular formation, various degrees of impaired consciousness (coma, stupor, stunning, akinetic mutism) are often observed.
The total defeat of the bridge is sometimes accompanied by the so-called locked-in syndrome - deafferentation syndrome, when the patient cannot move his limbs and speak, but he retains consciousness, eye movements and voluntary blinking, which undoubtedly facilitates the patient's contact with others.
This syndrome is a consequence of true paralysis of the limbs and anarthria as a result of bilateral damage to the motor and cortical-nuclear pathways.
11. Arteries of the medulla oblongata
Paramedian arteries in the oral part of the medulla oblongata depart from the vertebral arteries, in the caudal part - from the anterior spinal artery. They supply blood pyramidal path, medial loop, infranuclear fibers and the nucleus of the hypoglossal nerve. With a heart attack in this area, the so-called medial medulla oblongata syndrome occurs - paralysis of the hypoglossal nerve on the side of the focus
12. Inferior posterior cerebellar artery
The largest branch of the vertebral artery is the long circumflex artery for the medulla oblongata. It nourishes the retrolivar lateral sections of the medulla oblongata (rope body, the region of the vestibular nuclei, the descending nucleus and root of the trigeminal nerve, the spinothalamic pathway, the nuclei of the glossopharyngeal and vagus nerve) and the cerebellum. A heart attack in this area develops with blockage of the vertebral and inferior posterior cerebellar arteries, clinically it manifests itself as Wallenberg-Zakharchenko syndrome, which is a lateral syndrome of the medulla oblongata.
With damage to the lower sections of the brain stem and upper segments of the spinal cord, in the lateral columns of which the reticulospinal path passes, sometimes Undine's syndrome occurs (the name is taken from German mythology) - the loss of the ability to automatically breathe due to the dissociation of the respiratory center of the medulla oblongata with the spinal motor neurons of the respiratory muscles, while the the latter with the cerebral cortex remain intact. At the same time, breathing in the state of wakefulness is not disturbed, while in a dream, a severe violation of breathing occurs, up to its stop with a fatal outcome.
The spinal cord is supplied with blood by the anterior and two posterior spinal arteries. Between them there are anastomoses, through which segmental arterial rings are formed.
The spinal arteries receive blood from the radicular arteries. The superior system of radicular arteries gives off branches to the cervical and three upper thoracic segments of the spinal cord. The middle system of radicular arteries supplies blood to the thoracic segments IV through VIII. Lower system- Adamkevich's artery - supplies blood to the lower thoracic, as well as all lumbar and sacral segments of the spinal cord.
The outflow of blood from the spinal cord is carried out through the radicular veins. Through them, blood flows into the anterior and posterior vertebral plexuses. They are located between the sheets of the dura mater. From the venous plexuses, blood enters the cervical, vertebral, intercostal and lumbar veins. If the venous plexuses expand varicosely, then the spinal cord is compressed in the spinal canal.
Neurological symptoms in case of circulatory disorders in the basin of the anterior spinal artery depend on the level of the lesion. If the pathology is higher than the cervical thickening, then spastic tetraplegia develops, superficial sensitivity is disturbed, and central disorders of pelvic functions are observed. If the focus is located in the thoracic region, then spastic paraplegia of the legs is noted. If blood circulation in the basin of the posterior spinal artery is disturbed, then spastic paralysis, disorders of pelvic functions and a violation of deep sensitivity are noted. If Adamkevich's artery suffers, then paresis of the legs develops, sensitivity is disturbed, starting from the level of the X-XV thoracic segments, as well as incontinence or retention of stool and urine.
