Peripheral circulatory disorders treatment. Typical disorders of peripheral circulation and microcirculation. Cerebrovascular insufficiency.
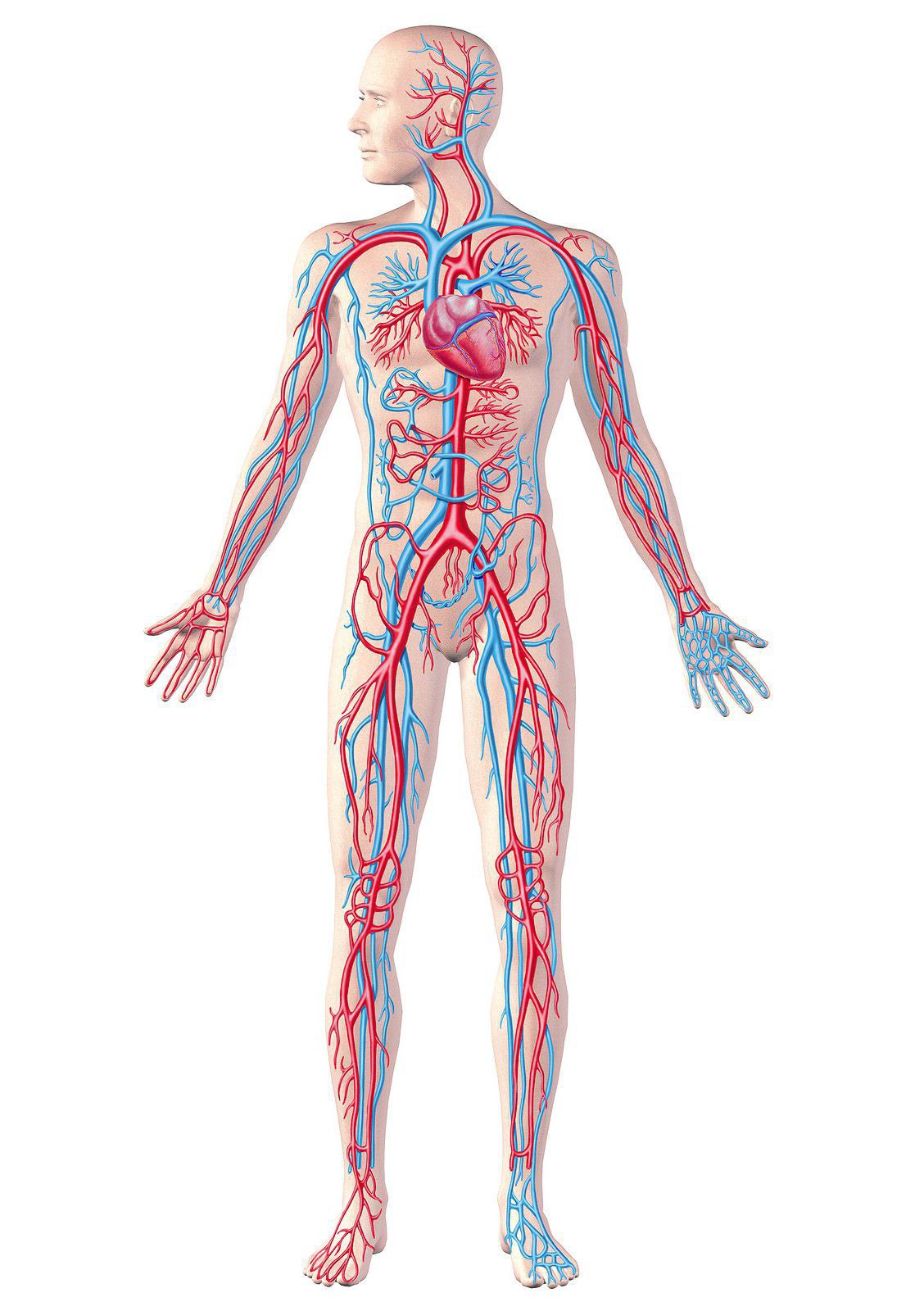
Blood circulation in the body is a continuous process. It is necessary to provide the organs and systems of the body with oxygen and nutrients. Also, with the help of the bloodstream, substances formed as a result of metabolic processes of cellular activity are also eliminated.
Poor blood circulation in the extremities is diagnosed when the vessels are unable to provide adequate nutrition to the tissues. This can be understood if there are characteristic symptoms: tingling in the fingers, numbness, trophic changes in the skin.
What medications can improve cerebral circulation?
Certain categories of medications take time to cure. The following changes occur at the reception. Eliminates free radicals that contribute to the destruction of cell walls. Improves blood flow to the brain.
- Fuel the growing nerve impulse.
- Improves attention and memory.
- There is better penetration and absorption of glucose into nerve cells.
- There is a recovery process after stroke and injury.
Circulatory disorders are divided into acute and chronic, slowly increasing. If you start treatment on time, noticing the first signs pathological changes vessels, blood supply function can be normalized.
Symptoms of peripheral circulatory disorders
On the signs poor circulation in the arms and legs the following factors indicate:
However, some medications to improve brain circulation can be taken without a doctor's prescription. Entry is limited to certain medications on expert advice and under your close supervision. The main means of this type are.
"Pantogam". Possible and over-the-counter medicine to take such remedies, improving cerebral blood flow. The list of drugs in this category is given above. The following medications should be required for negotiations. Satisfactory results give the drug an improvement cerebral circulation based on plant alkaloids such as vinca. This instrument has a type of antispasmodic effect and provides efficient expansion cerebral vessels and improved microcirculation in the vessels.
- the feeling of freezing of the limbs not only in the cold season, but also in the heat;
- crawling sensation;
- periodically there is a tingling sensation in the fingers;
- numbness of the limbs occurs;
- their hair begins to fall out;
- the skin color of the extremities becomes pale to blue;
- nails peel and often break;
- erectile function disappears;
- small wounds on the skin of the extremities take a long time to heal, begin to fester, and ulcers form.
Even with constant application of cream, the skin becomes dry, cosmetics the problem cannot be solved.
"Cinarizine" and "Nimodilin" - best medicine to improve cerebral circulation, at least affects the functionality of the main flow and acts exclusively in the brain area. There are tools of this nature. They will help you maintain long-term commitment to activities and distance mental problems with blood circulation in the brain. These active ingredients may include.
A drug such as Phezam has good reviews. Its action is vasodilating, antihypoxic, nootropic. Simple preventative medications include aspirin. Promotes good anticoagulants and reduces the formation of blood clots. Prescribe even with a very serious illness. However, you should pay attention to the fact that the base of the drug improves cerebral circulation - acetylsalicylic acid.
Poor blood circulation in the extremities is caused by the following reasons:
- Damage to blood vessels due to trauma
- Violation of the general diet.
- Smoking.
- Chronic illnesses that interfere with work endocrine system– for example, diabetes.
- Hypertonic disease.
- Violation biochemical composition blood, especially cholesterol levels.
Improve brain circulation
Fragility of blood vessels. As a result, it is very important to consult with your doctor to determine the necessary preventive doses. With this disease, unpleasant and sometimes even dangerous symptoms life and health. In this case, to help the patient resort to traditional medicine recipes.
For correct intake they must perform certain actions. You need to chop the periwinkle leaves. Then take a teaspoon herbal tea and fill with boiling water. After this, the composition should be placed on a small fire and brought to a boil. Boil for 5 minutes. Then we must add a tablespoon of hawthorn leaves and flowers and remove from the heat. Infuse the required portion for 2-3 hours. Then take half a glass of this composition before meals for 60 minutes. For achievement positive effect regular receipts necessary funds.
When initial symptoms poor blood circulation in peripheral organs, treatment must be started, otherwise the condition may cause unpleasant consequences.
Slow blood circulation increases the risk of trophic ulcers, can provoke the onset of a gangrenous state. Ulcers occur especially often in people with diabetes. Tight underwear, uncomfortable shoes– and the abrasion turns into a purulent-inflammatory process.
It is good to regulate cerebral hemodynamics. There are also unique criteria when preparing the drink. To do this, take a spray dry medicinal herb and pour boiling water over it. This composition infuses for 15 minutes. This is followed by your tension. Treatment should be carried out after 21 days. After receiving this extremely important means for adhesion - dosage.
Drink this drink on a specific occasion, that is, when a stroke occurs. In this case, there are two methods. Valerian root is filled with boiling water. This composition infuses for 8 hours. This drink is taken 3 times a day for 1 spoon of cannibal. You must also stick to the dose.
Most dangerous consequences– occurrence of critical ischemia lower limbs. A symptom of the disease is swelling of the fingers, which is difficult to eliminate.
Poor circulation in the hands indicates that the blood supply is compromised of cardio-vascular system. Numbness of the hands often appears against the background of pain in the chest, tingling of the heart, and during shortness of breath.
Alcoholic tincture of valerian is necessary at night to breathe. This procedure will lead to order nervous system and will help you sleep. The crushed Helenium root should be poured into a glass hot water. This composition should infuse for a day. Take the tincture before meals for thirty minutes a day, 4 times for 2 or 3 tablespoons.
In preparing this recipe as it is not difficult. A teaspoon of oregano was served in two cups boiled water. Take this drink in a cup at every meal. Crushed herb leaves Should be full of boiled water. The drink should be taken three times every other day using a glass.
A blood supply disorder is diagnosed based on clinical picture and special diagnostics.
Helps identify the problem following methods research:
- Ultrasound of veins and arteries;
- UZDS;
- CT scan;
- magnetic resonance imaging;
- contrast venography;
- scintigraphy.
The necessary examination methods are selected by the doctor based on the clinic and the patient’s capabilities. If the patient has a pacemaker, wave examinations are not performed.
Some action is required from the tool. They should then be rinsed thoroughly under running water. After that, they were crushed and vodka or alcohol was poured into them. The resulting composition insists on a 14-day period. To get this money, you need to dilute it for 1 hour. Therapy, in this case, the process continues for several weeks. Then a break was organized for a month.
The crushed leaves of this herb should be boiled in boiling water. Insist that the composition lasts 30 minutes. Use this food tool for 60 minutes in one article. You must also maintain certain proportions. Drink this drink within 30 minutes. Taking the necessary means to exercise 3 times a day. Namely, morning, noon and night for nine months. This drink provides memory retention.
Treatment of peripheral circulatory disorders
What to do if there are symptoms of poor circulation in the lower extremities? Most likely, this is the beginning of varicose veins and you should contact a phlebologist.
In order to stop the development of the disease, the following drugs are prescribed:

In this case, you need to mix ingredients such as speedwell, lemon balm, strawberry leaves, fruits and hawthorn flowers. Then first a spoonful of this compound is steamed with boiling water. You should eat your quota daily. Optionally, honey can be added. This prescription should be used when cerebral blood flow is impaired in the context of manifestations of atherosclerosis.
In this case, you need to chop 500 g of frozen blueberries. To this you need to add honey and grated horseradish root. This mix is a low mixer. After this, you need to pour it into jars and cool. The use of this food mixture occurs after taking it three times a day for 3 hours. With a spoon, drinking hot tea. The dose of honey can be increased to 500, using mixing vessels to strengthen, restore memory, stabilize cerebral circulation, and increase immunity.
- Venotonic drugs used orally and externally. They strengthen the venous walls and increase their tone.
- Heparin-containing drugs may also be local action and prescribed for internal use. With their help, the composition of the blood and its coagulability change.
- Venolife, a drug that combines the properties of heparin-containing and venotonic drugs, has proven to be effective. In addition, it contains vitamin B5. Venoline helps treat numbness, reduce swelling and relieve external manifestations disturbances in blood supply - and a change in its color. This quality of the drug is very much appreciated by women.
Massage and physiotherapy are included in the treatment of varicose veins: magnetic therapy, pneumocompression. Special compression garments help reduce pain
Means improvement of peripheral circulation
Let's look at this topic in detail. The following medicines for improvement peripheral circulation. These drugs help attract additional blood volumes from the intercellular spaces in the right direction. For example, the drugs “Reopoliglyukin” and “Reomacrodecs”.
They are called angioprotectors. They help normalize capillary permeability and improve metabolic processes in vascular walls. These tools help improve blood flow, microcirculation, and elasticity of red blood cells. These drugs also expand blood vessels, thereby reducing their resistance and peripheral blood pressure. They help improve microcirculation in the brain. Is there a cerebroprotective effect? Use these drugs to improve brain circulation, Cordafen, Cordaflex, Nimotop, Sinarizine, Logimax, Stugeron, Arifon, Adalat, Brainal, Cordipin, Grindeke Cortiazem Diacordin Nafadil Cinnasan Lacipil Norvax Nikkard » “Tsindil” “Foridon” “Nemotan” “Stamo” “Plendil”.
What to do if your hands constantly swell and hurt? The best remedy to combat hand numbness - underwater massage.
Traditional medicine in the treatment of peripheral blood supply
To combat impaired peripheral blood supply in the piggy bank traditional medicine there are many recipes.
The following procedure effectively helps restore blood supply to the arms and legs:
Medicines in this category dilate blood vessels, which leads to increased cerebral blood flow. They have very vascular spasms in the brain. This is an important feature. If atherosclerotic vessels are affected, the effectiveness of these agents is less pronounced. The disadvantage of these assets is the presence of the phenomenon of “theft”.
This refers to a type of natural raw material. The effects of drugs in this category, unlike synthetic drugs, develop much more slowly. In this case, the manifestation of the therapeutic effect is facilitated by the combination of certain compounds. Drugs in this group are effective for diseases of the cerebral vessels and manifestations of obliterating diseases of the lower extremities.

- mix sugar and sunflower oil in equal quantities;
- prepare a container with hot water, 250 ml – 2 tablespoons of table salt;
- Anoint the skin with a mixture of butter and sugar, lower the limb into saline solution– its initial temperature should be about 38ºС;
- keep the limb in water for 30-45 minutes.
This medicine will help restore blood supply to the legs and arms. A quarter-liter jar is filled with crushed garlic, filled with water and placed in a dark, cool place for 2 weeks. The composition must be stirred a couple of times a day. When the product is infused, it is filtered and placed in the refrigerator. Take 3 times a day, 5 drops, diluted in a tablespoon of water. The course of treatment is 10-14 days.
These funds promote the expansion of arterioles and veins, small venules. This provides a reduction blood pressure. Medicines in this category help improve blood flow through this environment, which increases the elasticity of red blood cells. They also ensure normalization of capillary blood flow.
They promote vasodilation, intestinal, kidney, skin, especially precapillaries and arterioles, which reduces overall resistance. This leads to better blood supply to peripheral tissues. This drug is “Prazosin”, “Sermion”, “Pirroxan”, “Nilogrin”, “Phentolamine”.
Another bath is herbal. It is made from equal parts of chamomile, nettle, oregano, and lemon balm. Pour 2 cups of herbal raw material into 3 liters of boiling water, wait until it cools down to 38ºC, and place your hands or feet in the bath.
Prevention of blood supply disorders

These drugs have a vasodilator effect. This is done by stimulating dopamine receptors. Drugs of this type help increase blood flow in the vessels located in the lower extremities. Conclusion After reading the above, everyone can learn about what remedies exist to improve cerebral circulation. The reference remedies listed in this document will help you solve the problem.
Increases the body's resistance to hypoxia, mainly brain tissue. It prevents the development of toxic or traumatic cerebral edema. Improves cerebral and peripheral blood circulation, improves blood rheology. Children under 12 years old. Hypersensitivity to medicine.
- Reduced blood clotting.
- Erosive sedation.
- Peptic ulcer and duodenum in the acute phase.
- Acute ischemic attacks.
- Acute myocardial infarction.
To improve the condition of the peripheral vessels of the extremities, they require dosed physical exercise. For the legs it is hiking at a moderate pace, for the arms - gymnastics. If you have to constantly type or do monotonous work, you need to stop every 45 minutes.
Must be followed special diet, bring the diet closer to the dietary table according to Pevzner No. 9 and 10. Limit alcohol consumption, try to get rid of smoking.
The tablets contain lactose, so the medicine is not recommended for patients with congenital galactosemia, glucose or galactose malabsorption, or congenital lactase deficiency. In the absence of sufficient data, the medicine should not be prescribed to children under 12 years of age.
The course of treatment is at least 8 weeks. The course of treatment is at least 6 weeks. The tablets should be taken with a small amount of liquid, tightly adjacent to water. The medicine is taken without food. In case of unavailability or if the drug was made in insufficient quantities, subsequent refills should be carried out as described in the regimen distribution without any changes.
The consequences of impaired peripheral blood supply are not only limitation of their function, pain during movement and at rest.
If a blood clot breaks off in the lower extremities, cerebral vessels may be damaged. And this is fraught with such serious illness like ischemic stroke.
PERIPHERAL CIRCULATION DISORDER
THROMBOSIS AND EMBOLISM
PLAN
1. The concept of peripheral circulation.
2. Arterial hyperemia.
2.1. Physiological hyperemia.
2.2. Pathological arterial hyperemia.
2.3. Neurogenic arterial hyperemia of the neurotonic type.
2.4. Neurogenic arterial hyperemia of the neuroparalytic type.
3. Venous hyperemia.
4. Ischemia.
4.1. Compressive ischemia.
4.2. Obstructive ischemia.
4.3. Angiospastic ischemia.
6. Thrombosis.
6.1. Definition of thrombosis.
6.2. The main factors of thrombosis.
6.3. Outcome of thrombosis.
7. Embolism.
7.1. Embolism of exogenous origin.
7.2. Embolism of endogenous origin.
7.2.1. Fat embolism.
7.2.2. Tissue embolism.
7.2.3. Amniotic fluid embolism.
7.3. Small embolism circle of blood circulation.
7.4. Embolism of the systemic circulation.
7.5. Portal vein embolism.
Blood circulation in the area of the peripheral vascular bed (small arteries, arterioles, capillaries, postcapillary venules, arteriovenular anastomoses, venules and small veins), in addition to blood movement, ensures the exchange of water, electrolytes, gases necessary nutrients and metabolites in the blood – tissue – blood system.
The mechanisms of regulation of regional blood circulation include, on the one hand, the influence of vasoconstrictor and vasodilator innervation, on the other, the effect on the vascular wall of nonspecific metabolites, inorganic ions, local biologically active substances and hormones brought by the blood. It is believed that with a decrease in the diameter of blood vessels, the importance of nervous regulation decreases, and metabolic regulation, on the contrary, increases.
In an organ or tissue, in response to functional and structural changes in them, local circulatory disorders may occur. The most common forms of local circulatory disorders: arterial and venous hyperemia, ischemia, stasis, thrombosis, embolism.
ARTERIAL HYPEREMIA.
Arterial hyperemia is an increase in the blood supply to an organ as a result of excess blood flow through the arterial vessels. It is characterized by a number of functional changes and Clinical signs:
diffuse redness, dilatation of small arteries, arterioles, veins and capillaries, pulsation of small arteries and capillaries,
· increase in the number of functioning vessels,
· local temperature increase,
· increase in the volume of the hyperemic area,
· increased tissue turgor,
increased pressure in arterioles, capillaries and veins,
· Accelerate blood flow, increase metabolism and enhance organ function.
The causes of arterial hyperemia can be: the influence of various environmental factors, including biological, physical, chemical; increased load on an organ or tissue area, as well as psychogenic effects. Since some of these agents are ordinary physiological stimuli (increased load on the organ, psychogenic effects), arterial hyperemia that occurs under their influence should be considered physiological. The main type of physiological arterial hyperemia is working, or functional, as well as reactive hyperemia.
Working hyperemia - this is an increase in blood flow in an organ, accompanying an increase in its function (hyperemia of the pancreas during digestion, skeletal muscle during its contraction, an increase in coronary blood flow with increased heart function, a rush of blood to the brain during mental stress).
Reactive hyperemia represents an increase in blood flow after its short-term restriction. It usually develops in the kidneys, brain, skin, intestines, and muscles. The maximum response is observed a few seconds after resumption of perfusion. Its duration is determined by the duration of the occlusion. Due to reactive hyperemia, the “debt” in blood flow that arose during occlusion is thus eliminated.
Pathological arterial hyperemia develops under the influence of unusual (pathological) stimuli ( chemical substances, toxins, products of impaired metabolism formed during inflammation, burns; fever, mechanical factors). In some cases, the condition for the occurrence of pathological arterial hyperemia is an increase in the sensitivity of blood vessels to irritants, which is observed, for example, with allergies.
Infectious rash, redness of the face with many infectious diseases, (measles, typhus, scarlet fever), vasomotor disorders with systemic lupus erythematosus, redness of the skin of an extremity when certain nerve plexuses are damaged, redness of half the face with neuralgia associated with irritation trigeminal nerve, etc., are clinical examples pathological arterial hyperemia.
Depending on the factor causing pathological arterial hyperemia, we can talk about inflammatory, thermal hyperemia, ultraviolet erythema, etc.
According to pathogenesis, two types of arterial hyperemia are distinguished - neurogenic (neurotonic and neuroparalytic type) and caused by the action of local chemical (metabolic) factors.
Neurogenic arterial hyperemia of neurotonic type may occur reflexively due to irritation of extero- and interoreceptors, as well as irritation of vasodilator nerves and centers. Mental, mechanical, temperature, chemical (turpentine, mustard oil, etc.) and biological agents can act as irritants.
A typical example of neurogenic arterial hyperemia is redness of the face and neck during pathological processes during internal organs(ovaries, heart, liver, lungs).
Arterial hyperemia, caused by the cholinergic mechanism (the influence of acetylcholine), is also possible in other organs and tissues (tongue, external genitalia, etc.), the vessels of which are innervated by parasympathetic nerve fibers.
In the absence of parasympathetic innervation, the development of arterial hyperemia is caused by the sympathetic (cholinergic, histaminergic and beta-adrenergic) system, represented in the periphery by the corresponding fibers, mediators and receptors (H2 receptors for histamine, beta-adrenergic receptors for norepinephrine, muscarinic receptors for acetylcholine).
Neurogenic arterial hyperemia of the neuroparalytic type can be observed in the clinic and in animal experiments during transection of sympathetic and alpha-adrenergic fibers and nerves that have a vasoconstrictor effect.
Sympathetic vasoconstrictor nerves are tonically active and in normal conditions constantly carry impulses of central origin (1-3 impulses per 1 second at rest), which determine the neurogenic (vasomotor) component of vascular tone. Their mediator is norepinephrine.
In humans and animals, tonic pulsation is inherent in the sympathetic nerves going to the vessels of the skin upper limbs, ears, skeletal muscles, alimentary canal, etc. Transection of these nerves in each of these organs causes an increase in blood flow in the arterial vessels. The use of periarterial and ganglion sympathectomy for endarteritis accompanied by prolonged vascular spasms is based on this effect.
Arterial hyperemia of the neuroparalytic type can also be obtained chemically by blocking the transmission of central nerve impulses in the area of the sympathetic nodes (using ganglion blockers) or at the level of sympathetic nerve endings (using sympatholytic or alpha-blocking agents). Under these conditions, voltage-dependent slow Ca 2+ channels are blocked, the entry of extracellular Ca 2+ into smooth muscle cells along the electrochemical gradient, as well as the release of Ca 2+ from the sarcoplasmic reticulum is disrupted. Contraction of smooth muscle cells under the influence of the neurotransmitter norepinephrine thus becomes impossible. The neuroparalytic mechanism of arterial hyperemia partially underlies inflammatory hyperemia, ultraviolet erythema, etc.
The idea of the existence of arterial hyperemia (physiological and pathological), caused by local metabolic (chemical) factors, is based on the fact that a number of metabolites cause vasodilation, acting directly on the non-striated muscle elements of their walls, regardless of innervation influences. This is also confirmed by the fact that complete denervation does not prevent the development of either working, reactive, or inflammatory arterial hyperemia.
Important role the increase in blood flow during local vascular reactions is attributed to changes in the pH of the tissue environment - a shift in the reaction of the environment towards acidosis promotes vasodilation due to an increase in the sensitivity of smooth muscle cells to adenosine, as well as a decrease in the degree of oxygen saturation of hemoglobin. Under pathological conditions (burn, injury, inflammation, exposure to UV rays, ionizing radiation, etc.), along with adenosine, other metabolic factors also become significant.
The outcome of arterial hyperemia may be different. In most cases, arterial hyperemia is accompanied by increased metabolism and organ function, which is an adaptive reaction. However, adverse consequences are also possible. In atherosclerosis, for example, a sharp dilation of a vessel may be accompanied by rupture of its wall and hemorrhage into the tissue. Such phenomena are especially dangerous in the brain.
VENOUS HYPEREMIA.
Venous hyperemia develops due to an increase in blood supply to an organ or tissue area as a result of obstructed blood outflow through the veins.
Reasons for its development:
· blockage of veins by a thrombus or embolus;
· compression by a tumor, scar, enlarged uterus, etc.
Thin-walled veins may also be compressed in areas sharp increase tissue and hydrostatic pressure (at the site of inflammation, in the kidneys with hydronephrosis).
In some cases, the predisposing factor of venous hyperemia is the constitutional weakness of the elastic apparatus of the veins, insufficient development and reduced tone of the smooth muscle elements of their walls. Often this predisposition is familial in nature.
Veins, like arteries, although to a lesser extent, are rich reflexogenic zones, which suggests the possibility of a neuro-reflex nature of venous hyperemia. The morphological basis of vasomotor function is the neuromuscular apparatus, which includes smooth muscle elements and effector nerve endings.
Venous hyperemia also develops when the function of the right ventricle of the heart weakens, the suction action decreases chest (exudative pleurisy, hemothorax), obstruction of blood flow in the pulmonary circulation (pneumosclerosis, emphysema, weakened left ventricular function).
The main factor causing local changes in venous hyperemia is oxygen starvation (hypoxia) of the tissue.
Hypoxia in this case is initially caused by limited influx arterial blood, then the effect on tissue enzyme systems of metabolic products, resulting in a violation of oxygen utilization. Oxygen starvation with venous hyperemia causes disruption of tissue metabolism, causes atrophic and dystrophic changes and excessive growth of connective tissue.
Along with local changes in venous hyperemia, especially if it is caused common reasons and is of a generalized nature; a number of general hemodynamic disorders with very serious consequences are also possible. Most often they occur when large venous collectors are blocked - the portal vein, the inferior vena cava. The accumulation of blood in these vascular reservoirs (up to 90% of all blood) is accompanied by a sharp decrease in blood pressure and disruption of nutrition of vital organs (heart, brain). Death may occur due to heart failure or respiratory paralysis.
A disturbance of peripheral circulation, which is based on a limited or complete cessation of arterial blood flow, is called ischemia (from the Greek ischeim - to delay, stop, haima - blood) or local anemia.
Ischemia is characterized by the following symptoms:
blanching of the ischemic area of the organ;
· decrease in temperature;
· disturbance of sensitivity in the form of paresthesia (feeling of numbness, tingling, “crawling”);
· decrease in blood flow speed and organ volume;
· decreased blood pressure at the artery site;
located below the obstacle, a decrease in oxygen tension in the ischemic area of the organ or tissue;
· impaired formation of interstitial fluid and decreased tissue turgor;
· dysfunction of an organ or tissue;
· dystrophic changes.
The cause of ischemia can be various factors: compression of the artery; obstruction of its lumen; effect on the neuromuscular apparatus of its wall. In accordance with this, compression, obstructive and angiospastic types of ischemia are distinguished.
Compressive ischemia occurs from compression of the adductor artery by a ligature, scar, tumor, foreign body and etc.
Obstructive ischemia is a consequence of partial narrowing or complete closure of the artery lumen by a thrombus or embolus. Productive-infiltrative and inflammatory changes in the artery wall that occur with atherosclerosis, obliterating endarteritis, periarteritis nodosa, also lead to limitation of local blood flow as obstructive ischemia.
Angiospastic ischemia occurs as a result of irritation of the vasoconstrictor apparatus of blood vessels and their reflex spasm caused by emotional influence (fear, pain, anger), physical factors(cold, injury, mechanical irritation), chemical agents, biological irritants (bacterial toxins), etc. In pathological conditions, vasospasm is characterized by a relative duration and significant severity, which can cause a sharp slowdown in blood flow, even stopping it completely. Most often, vasospasm develops in arteries of relatively large diameter inside the organ, vascular type unconditioned reflexes from the corresponding interoreceptors. These reflexes are characterized by significant inertia and autonomy.
The nature of metabolic, functional and structural changes in the ischemic area of tissue or organ is determined by the degree oxygen starvation, the severity of which depends on the rate of development and type of ischemia, its duration, location, nature of collateral circulation, functional state organ or tissue.
Ischemia that occurs in areas of complete obstruction or compression of the arteries, other things being equal, causes more severe changes than with spasm. Rapidly developing ischemia, like long-term ischemia, is more severe compared to slowly developing or short-term ischemia. Sudden tissue obstruction is especially important in the development of ischemia, since this may result in a reflex spasm of the branching system of a given artery.
Ischemia of vital organs (brain, heart) has more severe consequences than ischemia of the kidneys, spleen, lungs, and ischemia of the latter is more severe compared to ischemia of the skeletal, muscular, bone or cartilage tissue. These organs are characterized high level energy metabolism, at the same time, their collateral vessels are functionally absolutely or relatively unable to compensate for circulatory disorders. On the contrary, skeletal muscles and especially connective tissue, thanks to low level energy metabolism in them are more stable under ischemic conditions.
Stasis is a slowing down and stopping of blood flow in capillaries, thin arteries and veins.
There are true (capillary) stasis, which occurs as a result of pathological changes in the capillaries or disruption rheological properties blood, ischemic - due to the complete cessation of blood flow from the corresponding arteries into the capillary network and venous.
Venous and ischemic stasis are a consequence of a simple slowdown and cessation of blood flow. These conditions arise for the same reasons as venous hyperemia and ischemia. Venous stasis can be the result of compression of the veins, blockage by a thrombus or embolus, and ischemic stasis can be a result of spasm, compression or blockage of the arteries. Elimination of the cause of stasis leads to the restoration of normal blood flow. On the contrary, the progression of ischemic and venous stasis contributes to the development of true.
With true stasis, the column of blood in the capillaries and small veins becomes motionless, the blood is homogenized, red blood cells swell and lose a significant part of their pigment. The plasma, together with the released hemoglobin, goes beyond the vascular wall. In the tissues of the focus of capillary stasis there are signs of severe malnutrition and necrosis.
The cause of true stasis there may be physical (cold, heat), chemical (poisons, concentrated solution of sodium chloride, other salts, turpentine, mustard and croton oils) and biological (microorganism toxins) factors.
The mechanism of development of true stasis explained by intracapillary aggregation of erythrocytes, i.e. their gluing and formation of conglomerates, impeding blood flow. This increases peripheral resistance.
In the pathogenesis of true stasis, slowing down of blood flow in capillary vessels due to blood thickening is important. The leading role here is played by the increased permeability of the walls of capillary vessels located in the zone of stasis. This is facilitated etiological factors, causing stasis, and metabolites formed in tissues. Particular importance in the mechanism of stasis is given biologically active substances(serotonin, bradykinin, histamine), as well as an acylotic shift in the tissue reaction of the medium and its colloidal state. As a result, there is an increase in the permeability of the vascular wall and dilation of blood vessels, leading to blood thickening, slowing of blood flow, aggregation of red blood cells and, as a result, stasis.
Particularly important is the release of plasma albumin into the tissue, which helps to reduce the negative charge of erythrocytes, which may be accompanied by their loss from a suspended state.
Thrombosis is a process of intravital formation on inner surface the walls of blood vessels are blood clots consisting of its elements.
Blood clots can be parietal (partially reduce the lumen of blood vessels) or obstructive. The first type of blood clots most often occurs in the heart and trunks great vessels, the second - in small arteries and veins.
Depending on which components predominate in the structure of the blood clot, white, red and mixed blood clots are distinguished. In the first case, the thrombus is formed by platelets, leukocytes, and also a small amount of plasma proteins; in the second - red blood cells held together by fibrin threads; mixed thrombi are alternating white and red layers.
The main factors of thrombus formation (in the form of Vikhrov’s triad).
1. Damage to the vascular wall that occurs under the influence of physical forces (mechanical trauma, electricity), chemical (NaCl, FeCl3, HgCl2, AgNO3) and biological (endotoxins of microorganisms) factors as a result of disturbances in its nutrition and metabolism. These disorders are also accompanied by atherosclerosis, hypertonic disease, allergic processes.
2. Violation of the activity of the blood coagulation and anticoagulation system of the vascular wall. An increase in the activity of the blood coagulation system due to an increase in the concentration of procoagulants in it (thrombin, thromboplastin), as well as a decrease in the activity of the anticoagulant system (a decrease in the content of anticoagulants in the blood or an increase in the activity of their inhibitors), as a rule, leads to intravascular blood coagulation (IBC). VSSK is caused by a rapid and significant entry into the vascular bed of blood coagulation factors (tissue thromboplastin), which is observed with premature placental abruption, amniotic fluid embolism, traumatic shock, acute massive hemolysis of erythrocytes. The transition of VSSK to thrombosis occurs under the influence of coagulation factors of the vascular wall and platelets when they are damaged.
3. Slowing of blood flow and its disturbances (turbulence in the area of the aneurysm). This factor is probably of less importance, but it helps explain why blood clots form in veins 5 times more often than in arteries, in the veins of the lower extremities 3 times more often than in the veins of the upper extremities, as well as the high incidence of thrombosis during decompensation blood circulation, long-term bed rest.
The consequences of thrombosis can be different. Considering its importance as a hemostatic mechanism in acute injury accompanied by bleeding, thrombosis should be considered from a general biological point of view as an adaptive phenomenon.
At the same time, thrombus formation during various diseases(atherosclerosis, diabetes etc.) may be accompanied by severe complications caused acute disorder blood circulation in the area of the thrombosed vessel. The development of necrosis (infarction, gangrene) in the basin of a thrombosed vessel is the final stage of thrombosis.
The outcome of thrombosis can be aseptic (enzymatic, autolytic) melting, organization (resorption with replacement connective tissue), recanalization, septic (purulent) melting. The latter is especially dangerous, as it contributes to septicopyemia and the formation of multiple abscesses in various organs.
Embolism (from the Greek emballein - throw inside) is a blockage of blood vessels by bodies (emboli) brought by the blood or lymph flow.
Depending on the nature of the emboli, embolism is distinguished:
· endogenous, caused by a blood clot, fat, various tissues, amniotic fluid, gas (with decompression sickness).
Embolism is classified according to location:
systemic circulation,
· pulmonary circulation;
Portal vein system.
In all cases, the movement of emboli is usually carried out in accordance with the natural forward movement of blood.
Embolism of exogenous origin. Air embolism occurs when large veins are injured (jugular, subclavian, solid sinuses) meninges), which fall slightly and the pressure in which is close to zero or negative. This circumstance can also cause air embolism during medical procedures - when infusion of solutions into these vessels. As a result, air is sucked into the damaged veins, especially at the height of inspiration, with subsequent embolism of the vessels of the pulmonary circulation. The same conditions are created when the lung is injured or has destructive processes in it, as well as when pneumothorax is applied. In such cases, however, embolism of the vessels of the large circulation occurs. Receipt leads to similar consequences large quantity air from the lungs into the blood when exposed to explosive shock wave(air, water), as well as during “explosive decompression” and rapid ascent to high altitudes. The resulting sharp expansion of the pulmonary alveoli, rupture of their walls and the entry of air into the capillary network lead to inevitable embolism of the vessels of the systemic circulation. With anaerobic (gas) gangrene, gas embolism is also possible.
The sensitivity of different animals and humans to air embolism varies. The rabbit dies from intravenous administration 2-3 ml of air, dogs tolerate air injections in a volume of 50-70 ml/kg. Man in this regard occupies an intermediate position.
Embolism of endogenous origin. The source of thromboembolism is a particle of a detached thrombus. The separation of a blood clot is considered a sign of its inferiority (“sick blood clot”). In most cases, “sick blood clots” form in the veins of the systemic circulation (veins of the lower extremities, pelvis, liver), which explains the high frequency of pulmonary embolism. Only when blood clots form in the left half of the heart (with endocarditis, aneurysm) or in the arteries (with atherosclerosis) does embolism occur in the vessels of the systemic circulation. The reason for the inferiority of a blood clot, the detachment of its particles and thromboembolism is its aseptic or purulent melting, a violation of the retraction phase of thrombus formation, as well as blood coagulation.
Fat embolism occurs when drops of fat, most often of endogenous origin, enter the bloodstream. The cause of fat droplets entering the bloodstream is damage (crushing, severe concussion) to the bone marrow, subcutaneous or pelvic tissue and fat accumulations, and fatty liver.
Since the source of embolism is located primarily in the veins of the systemic circulation, fat embolism is possible primarily in the vessels of the pulmonary circulation. Only later is it possible for fatty droplets to penetrate through the pulmonary capillaries (or arteriovenous anastomoses of the pulmonary circulation) into the left half of the heart and the arteries of the systemic circulation.
The amount of fat causing fatal fat embolism varies in different animals within the range of 0.9-3 cm 3 /kg.
Tissue embolism observed in case of injury, when scraps of various body tissues, especially those rich in water, are possible ( Bone marrow, muscles, brain, liver) into the blood circulation system, especially the pulmonary circulation. Of particular importance is vascular embolism by cells malignant tumors, since it is the main mechanism for the formation of metastases.
Amniotic fluid embolism occurs when amniotic fluid enters damaged vessels of the uterus during childbirth in the area of the separated placenta.
Gas embolism is the main pathogenetic link in the state of decompression, in particular decompression sickness. Drop atmospheric pressure from increased to normal (for divers) or vice versa from normal to sharply decreased (rapid rise to altitude, depressurization of the aircraft cabin) leads to a decrease in the solubility of gases (nitrogen, oxygen, carbon dioxide) in tissues and blood and blockage of bubbles of these gases (firstly turn of nitrogen) capillaries located mainly in the systemic circulation basin.
Embolism of the pulmonary circulation. The most important functional change in vascular embolism of the pulmonary circulation is a sharp decrease in blood pressure in the systemic circulation and an increase in pressure in the pulmonary circulation.
There are several hypotheses explaining the mechanisms of the hypotensive effect in pulmonary embolism. There is a widespread opinion that acute decline blood pressure is considered as reflex hypotension (Schwingk-Parin unloading reflex). It is believed that the depressor reflex is caused by irritation of receptors located in the bed of the pulmonary artery.
A certain importance in lowering blood pressure during pulmonary embolism is given to weakening of heart function due to myocardial hypoxia, which is the result of an increased load on the right half of the heart and sharp decline blood pressure.
The obligatory hemodynamic effect of vascular embolism in the pulmonary circulation is an increase in blood pressure in the pulmonary artery and a sharp increase in the pressure gradient in the pulmonary artery-capillary area, which is considered as a result of a reflex spasm of the pulmonary vessels.
Embolism of the systemic circulation. As mentioned above, vascular embolism of the systemic circulation is most often based on pathological processes in the left half of the heart, accompanied by the formation of blood clots on its inner surface (thromboendocarditis, myocardial infarction), thrombus formation in the arteries of the systemic circulation followed by thromboembolism, gas or fat embolism. Places of frequent localization of emboli are the coronary, middle cerebral, internal carotid, and renal splenic arteries. All other things being equal, the localization of emboli is determined by the angle of origin of the lateral vessel, its diameter, and the intensity of blood supply to the organ. A large angle of origin of the lateral branches in relation to the upstream segment of the vessel, their relatively large diameter, and hyperemia are factors predisposing to one or another localization of emboli.
With gas embolism accompanying decompression sickness or “explosive decompression,” a predisposing factor to the localization of emboli in the vessels of the brain and subcutaneous tissue is the good solubility of nitrogen in lipid-rich tissues.
Portal vein embolism. Portal vein embolism, although much less common than embolism of the pulmonary and systemic circulation, attracts attention with its characteristic clinical symptom complex and extremely severe hemodynamic disturbances.
Due to the large capacity of the portal bed, blockage of the main trunk of the portal vein or its main branches by an embolus leads to an increase in blood supply to the organs abdominal cavity(stomach, intestines, spleen) and the development of portal hypertension syndrome (increased blood pressure in the portal vein system from 8-10 dollars to 40-60 cm water column). In this case, as a consequence, a characteristic clinical triad develops (ascites, expansion of the superficial veins of the anterior abdominal wall, enlargement of the spleen) and a number of general changes caused by circulatory disorders (decreased blood flow to the heart, stroke and minute volume of blood, decreased blood pressure), respiration (shortness of breath, then a sharp decrease in breathing, apnea) and functions of the nervous system (loss of consciousness, respiratory paralysis).
At the heart of these general violations lies predominantly in the decrease in the mass of circulating blood caused by its accumulation (up to 90%) in the portal bed. Such hemodynamic disturbances are often the direct cause of death in patients.
Literature.
1. N.N. Zaiko. Pathological physiology - K., 1985.
2. A.D.Ado, L.M.Ishimova. Pathological physiology - Medicine, 1980.
3. G.E. Arkadyeva, N.N. Petrintseva. Mechanisms of impaired platelet-vascular hemostasis - L., 1988.
4. V.S.Paukov, N.K.Khitrov. Pathology - M.: Medicine, 1989.
