Name acute disorders of the peripheral circulation. Violation of the peripheral circulation. Patients with acute ischemia: a sharp decrease in blood flow to the limb with the threat of gangrene.
Pathologies of the circulatory organs, classified in pathophysiology as hemodiscirculatory processes, arise due to changes in the properties and volume of blood in the vascular bed. In some pathologies of the circulatory system, the blood goes beyond the vessels. The main types of circulatory disorders, in addition to hyperemia, ischemia and stasis, include sludge, thrombosis and embolism.
Its origin lies in the discoordination of the functions of the coagulation and anticoagulation blood systems responsible for hemostasis. In many cases, the cause of disseminated intravascular coagulation is unknown. malignant tumor. Acute leukemia promyelocyte.
Metastatic cancer, most often adenocarcinoma. Blood clots are especially common in the microvessels of the lungs, kidneys, liver, adrenal glands, pituitary gland, brain, gastrointestinal tract, skin and in combination with multiple hemorrhages, dystrophy and necrosis of organs and tissues. You should be aware that in some cases at autopsy, due to the parallelism and the predominant action of the fibrinolytic system, microthrombi cannot be detected.
Arterial and venous circulation disorders: symptoms and causes
Pathologies such as circulatory disorders are divided into central, developing as a result of heart pathology, and peripheral, arising from vascular pathology.
Major violations peripheral circulation are:
Shock of the clinical state associated with a decrease in effective cardiac output, a violation of the autoregulatory microcirculatory system and is characterized by a generalized decrease in tissue blood supply, which leads to destructive changes internal organs. Based on the characteristics of the etiology and pathogenesis, the following types of hypovolemic shock are distinguished: neurogenic, septic, cardiogenic and anaphylactic.
Local circulatory disorders. Classification Local circulatory disorders are: - blood hyperemia, - venous hyperemia, - stagnant blood, - bleeding and hemorrhage, thrombosis, - embolism, - ischemia, - heart attack. Local blood hyperemia Local blood hyperemia is an increase in arterial blood flow to an organ or tissue.
- hyperemia (arterial and venous) - an increase in blood supply to the tissue;
- ischemia - a decrease in blood supply to an organ or tissue;
- stasis - cessation of blood flow in organs and tissues.
Circulatory disorders can be arterial and venous in nature.
Arterial hyperemia
Arterial hyperemia- this is an increase in the blood filling of an organ due to an increase in the amount of blood flowing through its dilated vessels. There are physiological hyperemia, which occurs normally with increased organ function, as well as reflex under the influence of ultraviolet rays, cold, heat, etc., and pathological hyperemia, which occurs in the following cases:
There are physiological and pathological hyperemia. An example of physiological arterial hyperemia can be a shame of shame on the face, pink and red skin at the site of its thermal or mechanical irritation. Based on the etiology and mechanisms of development, the following types of abnormal arterial hyperemia are distinguished. Angioedema has been observed in vasomotor disorders caused by irritation of the vasodilating nerves, or paralysis of the vasoconstrictive nerves, irritating the sympathetic ganglia.
Examples of such disorders are acute lupus erythematosus, in which there is hyperemia of the area in the form of symmetrical lying butterflies on the face or reddening of the face and conjunctiva of the eye with many acute infections. Angioedema includes hyperemia of the extremities in case of damage to the corresponding nerve plexuses, hyperemia of half of the persons with neuralgia associated with stimulation trigeminal nerve etc.
- with inflammation;
- rapid decompression of compressed vessels (for example, when emptying abdominal cavity from the accumulation of ascitic fluid);
- creating a rarefied space (vacant hyperemia) - for example, when using medical cups;
- overload or drug blockade of vasoconstrictors sympathetic nerves(neuroparalytic hyperemia).
Clinically, such a circulatory disorder as arterial hyperemia is manifested by reddening of the tissues and a local increase in their temperature.
Causes of acute and chronic circulatory disorders
Angioedema hyperemia is characterized by an acceleration of blood flow not only in general functioning, but also in the capillaries opening the reserve. The skin and mucous membranes become red, slightly swollen when touched warm or hot. Usually this hyperemia passes quickly and leaves no traces.
Congestive accumulation occurs in conditions of closure of the main artery, for example, an atherosclerotic plaque. Rich blood is rushed into the collaterals, which expand. Of great importance in the development of secondary arterial hyperemia, under equal other conditions, is the rate of closure of the main vessel and the level blood pressure. Stenosis and even closure of large arteries, when they develop over the years, may not be accompanied by serious consequences. This is due to the fact that collaterals in the arterial system develop in parallel with the growth of blood flow obstructions in the course of the main trunk.
Venous congestion
Venous (congestive) hyperemia- an increase in the blood filling of a tissue area with a decrease in the amount of flowing blood.
The causes of such circulatory disorders as venous hyperemia are:
- thrombosis or compression of the veins from the outside (tumor, scars, pregnant uterus, during surgical ligation of the vessel);
- stagnation and slowing of blood flow in the veins of the lower body with a decrease in the pumping function of the heart (right ventricular heart failure);
- blood stasis in lower limbs in people who work standing for a long time.
Clinical symptoms of circulatory disorders venous hyperemia are cyanotic coloration of tissues, or cyanosis, and pathology may be accompanied by edema.
Means for improving peripheral circulation
Sometimes, for example, with atherosclerosis, the closure of both coronary arteries heart is not accompanied by severe symptoms of heart failure, since it develops collateral circulation due to the mediastinum, interortal, pericardial and bronchial arteries. Knowledge of the anatomical possibilities of collateral circulation allows surgeons to successfully perform operations by ligating the femoral, popliteal, carotid arteries no development severe complications in the form of necrosis of the corresponding organs.
Pathologies of the circulatory system: stasis and sludge
Also, pathologies of the peripheral circulation include such disorders as stasis and sludge.
Stasis
Stasis- this is a type of circulatory disorder in which there is a local stop of blood flow in small vessels, mainly capillaries.
The cause of this circulatory disorder is the complete cessation of blood flow. Also, stasis can occur due to a sharp violation of the outflow of blood, as well as due to various diseases of an inflammatory and non-inflammatory nature (true capillary stasis), leading to intracapillary crowding (aggregation) of red blood cells and stopping capillary blood flow.
Postanemic hyperemia develops when the factor causing local anemia is rapidly removed. Vessels, previously dried with a dry cloth, expand sharply and fill with blood. The danger of such arterial hyperemia lies in the fact that overfilled vessels, especially in the elderly, can rupture, which leads to bleeding and hemorrhage. In addition, due to a sharp redistribution of blood, there may be a lack of erythrocytes from other organs, such as the brain, which in the clinic are accompanied by the development of syncope.
Stasis can be reversible or irreversible (in this case, the blood flow is not restored, and necrosis occurs in the corresponding tissue area). Outward manifestation such a circulatory disorder is a "marble" color on the skin.
Sludge
Sludge (sludge syndrome)- this is a state of the blood, which is based on the aggregation (clumping) of red blood cells (their extreme degree of aggregation). With sweetness, the boundaries between individual erythrocytes become poorly distinguishable.
Therefore, manipulations such as removing fluid from chest and abdominal cavity are produced slowly. An example of such a set of hyperemia of the skin under the influence of medical cupping. Inflammatory hyperemia is one of the important clinical signs any inflammation.
Hyperemia based on an arteriovenous shunt occurs when an anastomotic wound forms between an artery and a vein, and arterial blood thrown into a vein. The danger of this hyperemia is determined by the possibility of division of the anastomosis and the development of bleeding.
Local venous hyperemia. Local venous congestion develops when the outflow of venous blood from the body or parts of the body is disturbed. Based on the etiology and mechanisms of development, there are: - obstructive venous congestion caused by blockage of the lumen of a vein thrombus, embolus; - venous hyperemia of the compressor, observed when the veins are compressed from external inflammatory edema, edema, ligature and growing connective tissue; - secondary venous hyperemia, which can be observed when a large trunk of the venous trunk is closed, for example, a porto-caval anastomosis due to the difficulty of blood flow in the portal vein.
The main features of blood slugging are the adhesion of formed elements to each other and the increase in plasma viscosity, which leads to such a state of blood, in which its flow through small-caliber vessels is difficult.
Manifestations of circulatory disorders: ischemia
 Speaking about the symptoms and causes of circulatory disorders, ischemia is considered separately.
Speaking about the symptoms and causes of circulatory disorders, ischemia is considered separately.
Obesity and physical inactivity are common risk factors for atherosclerosis
Morphological restructuring of venous collaterals occurs according to the same principle as arterial, however, taking into account the macroscopic difference in that the expansion of venous vessels takes on serpentine and angular forms. Such changes are called varicose veins, which can be seen on the lower extremities, in the root of the seeds, in the wide ligaments of the uterus, in the urethra, in the area anal openings and the nearby part of the rectum - Called hemorrhoids. The veins on the anterior abdominal wall are full blood vessels of this type, known in literature as the "head of Medusa", referring to the hair of Medusa Gorgon from Greek mythology.
Ischemia is a reduced blood supply to a tissue area due to a weakening or cessation of blood flow to it through the arteries.
Causes of ischemia:
- compression of an artery (by tourniquet, tumor, scar, foreign body, surgical ligation of the vessel);
- blockage of the artery (thrombus, embolism, narrowing of the lumen of the artery in vascular diseases);
- reflex ischemia (pain, visual, sound, chemical, emotional stimuli, etc.).
Clinical manifestations of ischemia depend on the location of the ischemic area. So, a sign of circulatory disorders ischemia of the limbs is their blanching, numbness, "goosebumps", pain, limb function is impaired. With ischemia of the heart muscle, pain occurs, and with cerebral ischemia, this or that neurological symptomatology occurs.
Overflowing blood collateral veins expand dramatically, and the wall depletes them. This could be the reason dangerous bleeding. Varicose veins of the lower extremities are cyanosis, edema, pronounced atrophic processes: skin and subcutaneous tissue, especially the lower third of the splint, is very thin and the Xing ulcers that occur then can be healed with great difficulty. Local venous hyperemia is a reversible process if the cause is timely correction.
Stasis slows down to a stop, the blood flow in the microcirculation vessels, mainly in the capillaries. The remaining blood may be preceded by venous congestion or ischemia. However, this can occur without previous circulatory disorders, under the influence of endo- and exogenous causes, as a result of infections, various chemical and physical agents on the tissue, which leads to disruption of microcirculation innervation, with infectious - allergic and autoimmune diseases etc.
The outcomes of ischemia depend not only on localization, but also on the diameter of the closed vessel and on the degree of development of collateral (roundabout) circulation in this area. With a favorable outcome, the blood supply to the ischemic area is restored, with an unfavorable outcome, a site of tissue necrosis occurs - a heart attack. Distinguish: white heart attack that occurs in the myocardium, kidney, brain; red infarction, when the dead tissue area is soaked venous blood penetrating through highly permeable vascular walls (may occur in the lung, brain, in the intestinal wall); a white infarction with a hemorrhagic corolla, in which the white zone of necrosis is surrounded by a zone of hemorrhage due to the fact that the spasm of the vessels on the periphery of the infarction is replaced by their expansion with blood leaking through their walls.
Blood stasis is characterized by the arrest of blood in the capillaries and venules with an increase in the gap and agglutination of red blood cells in uniform postures - this is what distinguishes the stagnation of venous hyperemia. Hemolysis and blood clotting when this does not occur. Stasis must be distinguished from "silt-phenomenon". Sludge is a phenomenon of erythrocytes sticking together not only in capillaries, but also in vessels of different calibers, including veins and arteries. This syndrome is also the name of intravascular erythrocyte aggregation, observed with various infections, as a result of intoxication, the adhesion of erythrocytes, changes in their charge increased.
The usefulness of the collateral (roundabout) circulation depends on anatomical features blood supply to the ischemic area (main or branched type of blood supply), conditions vascular wall, the state of cardiac activity and nervous regulators of blood circulation. There are functionally absolutely sufficient and functionally insufficient (absolutely and relatively) collaterals. This, accordingly, affects the nature of the outcome of ischemia.
Since the process of local sludge develops in the pulmonary veins, for example, in the so-called shock lung or acute respiratory failure in adults. When various hypoxic origins can be isolated spasm of the vein, the so-called "venous crisis" on the Ricker. This can lead to the accumulation of granulocyte leukostasis inside the vascular bed: in venules and capillaries. Leukostasis is often associated with shock and is accompanied by leukodepidesis.
Stasis is a reversible phenomenon. Stasis is accompanied degenerative changes in the organs where it is observed. Irreversible stagnation leads to necrosis. Clinical Significance the eye is determined by the frequency of this phenomenon. Stasis and static marginal conditions are observed in angioedema, acute forms inflammation, shock, viral diseases such as influenza, measles. The most sensitive to circulatory disorders and hypoxia are the cerebral cortex. Stasis can lead to the development of a microinfarction.
Violation of the circulatory system: thrombosis and embolism
 Further, circulatory disorders such as thrombosis and embolism will be considered.
Further, circulatory disorders such as thrombosis and embolism will be considered.
Thrombosis
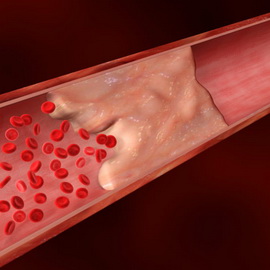
Thrombosis is called lifetime coagulation of blood or lymph in the lumen of the vessel with partial or complete blockage, leading to impaired blood flow.
Extensive stagnation in the focus of inflammation brings with it the danger of developing ossification tissue, which at the root can change its course. inflammatory process. For example, with pneumonia, which can lead to decay and the development of gangrene, that is, death.
thrombosis and embolism
From a biological point of view, stagnation is an adaptive mechanism of decompensation that underlies the regulation of peripheral circulation and blood supply to organs. Bleeding - the exit of blood from the lumen of the vessel or cavity of the heart. If blood spills into environment, then we are talking about external bleeding, if in the body cavity of the body - internal bleeding. Examples of external bleeding can be hemoptysis, nosebleeds, vomiting of blood, bleeding on the stool, bleeding from the uterus.
The mechanism of thrombus formation consists of combinations of three factors (Virchow's triad):
- slowing down of blood flow;
- damage to the vascular wall;
- increased blood clotting.
Vein thrombosis is also referred to as phlebothrombosis. If thrombosis is combined with inflammation of the vein wall, then they speak of thrombophlebitis. If there is a combination of arterial thrombosis with inflammation of its wall, this is called thromboarteritis. Symptoms of a circulatory disorder such as deep vein thrombosis are pain, swelling, and redness of the affected area.
Causes of circulatory disorders
If internal bleeding blood can accumulate in the pericardium, pleura, abdominal cavity. The withdrawal of blood outside the vascular bed with its accumulation in the tissue, called hemorrhage. Hemorrhage is a special type of bleeding. The causes of bleeding can be a gap, ulcers and increased permeability of the vessel walls.
Bleeding due to rupture of the walls of the vessel or heart - hemorrhage on rexin - occurs with necrosis, inflammation or sclerosis of the walls of the vessel or heart. Often there are ruptures of the aneurysm of the heart, aorta and arteries of the brain, pulmonary artery in vasculitis various etiologies, hypertension, atherosclerosis, etc.
Embolism
An embolism is a blockage of blood and lymphatic vessels particles carried by the blood or lymph. These particles are called emboli.
There are the following types of embolism:
- thromboembolism - embolism by a migrated fragment of a thrombus;
- tissue and cellular embolism - embolism with tissue sections in case of an organ injury, tumor cells, etc.;
- fat embolism - blockage of blood vessels with drops of fat, most often with fractures of long tubular bones;
- gas embolism (a variant of it is air embolism) - blockage of blood vessels by gas bubbles, for example, bubbles of nitrogen dissolved in the blood during decompression sickness in divers;
- bacterial embolism - blockage of blood vessels by conglomerates of bacteria during various diseases(for example, in acute hematogenous osteomyelitis);
- embolism by a foreign body (for example, a bullet, a shell fragment).
If the embolus, due to gravity, descends from top to bottom against the direction of blood flow, then they speak of a retrograde embolism. If the embolus venous system enters the arterial through an open septum between the left and right atrium, then this embolism is called paradoxical.
Thrombosis and embolism of arterial vessels lead to ischemia of the areas of blood supply by these vessels. venous thrombosis leads to venous congestion in zones venous outflow this vessel.
The fate of the thrombus may be different. A clot may grow over time. connective tissue(organization of a thrombus), partially or completely dissolve (recanalization of a thrombus), and also undergo purulent fusion.
The article has been read 1,553 times.
Violation of the peripheral arterial circulation most often develops in the lower extremities, which is associated with the peculiarities of the anatomy:the relative massiveness of the lower extremities requires blood supplylarge-caliber arteries with high blood pressure,which creates the prerequisites for the development of atherosclerosis, all other things being equal.
Narrowing of the arteries by atherosclerotic plaques leads to a progressive deficiency of blood flow, which in extreme cases results in the development of gangrene. The prevalence of atherosclerosis of the lower extremities according to epidemiological studies3% - 10% in the general populationwith an increase of up to 15% -20% in the subgroup of persons who have reached the age of 70 years.Risk of severe ischemialeading to gangreneis realized in approximately 4% of persons suffering from atherosclerosis of the arteries of the lower extremities.
Risk factors for the development of atherosclerosis of the arterieslower limbs:
Gender is a non-modifiable risk factor.Atherosclerosis develops more often and earlier in men. female hormones reduce the riskdevelopment of atherosclerosis in womenbefore the onset of menopause. However, drugs do not allow you to turn back time andhormone replacement therapy in the postmenopausal period in women does not improve, but worsens the prognosis in terms ofcardiovascular complications. On average, atherosclerotic lesions of the arteries of the lower extremities are 2 times more common in men.
Age. Most often, atherosclerosis develops in the elderly and old age after 70 years.
Smoking at least three times increases the risk of atherosclerotic lesions of the arteries of the lower extremities.
Arterial hypertension and diabetes 2-4 times increase the risk of atherosclerosis.
Dyslipidemia with elevated low-density lipoprotein levels2 times increases the likelihood of developing atherosclerosis.
obesity and low physical activity are common risk factors for atherosclerosis.
Hyperhomocyteinemia. An elevated level of homocysteine in the blood is determined in 1% of the general population, while in atherosclerosis of the arteries of the lower extremities, homocysteineincreased in 30% of cases.
Hypercoagulability. Several studies have shown an association between increased level fibrinogen in the blood and atherosclerotic lesions of the arteries of the lower extremities. An increase in hematocrit and blood viscosity in these patients is most often associated with smoking.
clinical picture.
Approximately 20% of people suffering from atherosclerosis of the arteries of the lower extremities do not complain. In 80% of cases, atherosclerotic lesions of the lower extremities occur with the development of various symptoms.
A typical symptom of atherosclerosis of the arteries of the lower extremities is intermittent claudication, which manifests itselfpain in calf muscles when walking,the pain disappears after a short rest. With the development of critical arterial stenosis, pain occurs at rest, trophic ulcers appear, and gangrene develops. Localizationstenosing lesion in the aorto-iliac segmentcauses pain syndrome in the gluteus area and in the hip area.
Some patients develop non-specific symptoms: discomfort in the lower extremities, cramps, weakness in the legs, decrease in the muscle mass of the lower extremities, erectile dysfunction in men, a decrease in hairline and thinning of the skin on the legs, a slowdown in nail growth, pallor of the skin of the legs,difficulty walking without typical symptoms intermittent claudication.
Diagnostics.
Diagnosis begins with detailing complaints, taking an anamnesis, assessing cardiovascular risk factorsand objective examination. On examination, attention is drawn to the atrophy of the muscles of the lower extremities, the weakening or absence of a pulse on palpation of the arteries of the lower extremities, and trophic changes in the skin.
Of great importance is the definition of the ankle-brachial index - the ratio of systolic blood pressure measured at the ankle and on the shoulder. Normal ankle-brachial index 1.0-1.4. A decrease in the ankle-brachial index below 0.9 is a criterion for obliterating atherosclerotic lesions of the arteries of the lower extremities.The most affordable and safe method for visualizing blood flow in the lower extremities– ultrasound dopplerography. More informative, but lessCT angiography and MRI angiography are dositukpronsmtyu.The most accurate imaging modality, invasive angiography with contrast injection into the femoral artery, is used in patients requiring surgery.
Treatment.
In the first place in the treatment of factor modificationcardiovascular risk: smoking cessation, blood pressure control, diabetes management, dyslipidemia control, healthy lifestyle life, intelligent physical exercise, restriction in the diet of animal fats, maintenance normal weight body.
Research showed high efficiency physiotherapy exercises, the ability to walk increased according to various sources by 50-200%, persons with intermittent lameness from physical education (treadmill) increased the distance traveled without pain by an average of 150 meters.
Pharmacological treatment:
Antiplatelet agents. Aspirinat a dose of 75-325 mg per day reduces the overall risk of death from vascular causes, the risk of myocardial infarction and stroke in patients suffering from atherosclerosis of the arteries of the lower extremities. In case of intolerance to aspirin, the appointment is consideredclopidlogrel I.
Naftidrofurylstudies have shown to increase the ability to walk without pain in patients with intermittent claudicationby about 25%. This drug is prescribed orally at 100-200 mg 2-3 times a day after meals.
Research has shown some efficiency L-carnitineand with symptoms of intermittent lameness. These substances are present on the pharmaceutical market mainly in the form of food additives.
Antihypertensive agents by themselves are not a treatment for atherosclerosis, but their appointment in hypertension favorably affects all outcomes of atherosclerotic vascular lesions. One large meta-analysis shows that prescribingACE inhibitorsbeneficial effect on the symptoms of intermittent claudication.
Purpose statinsbeneficial in terms of prevention of cardiovascular risks. One meta-analysis showed a symptomatic effect in intermittent claudication in the form of an increase in the duration of walking without pain by 163 meters.
Prostaglandin derivatives (alprostadil, iloprost) prevent the activation of leukocytes and platelets, protect the vascular endothelium, have a vasodilating effect.In critical ischemia, parenteralthe appointment of these drugs effectively improves blood circulation in the affected limbs. A number of studies have shown that the appointment of prostaglandin derivatives contributed to improved survival and increasedchance of saving a limb.
Pentoxifyllineis a derivative of methylxanthine chemically related to caffeine and theophylline molecules. Pentoxifyllinereduces the level of fibrinogen in the blood, improves rheological properties blood, has a vasodilatory effect. Pentoxifylline has a wide range pharmacological effects, with application points various fields medicine. The hepatoprotective effect is described, the effectiveness of pentoxifylline in alcoholic hepatitis and fatty hepatosis has been proven. This makes the appointment of pentoxifylline especially justified in the combination of peripheral arterial lesions with alcoholic or other liver damage. The effectiveness of pentoxifylline in diabetic nephropathy has been proven in terms of reducing proteinuria. The radioprotective effect of pentoxifylline has found its application in the prevention of a number of complications of radiation therapy - post-radiation fibrosis, radiation retinopathy. Pentoxifylline has found its use in hematology, it helps with anemia in people on hemodialysis.
Operative treatment. Surgical revascularization is necessary:
1. Patients with symptoms of intermittent claudication cannot be controlled with medication.
2. Patients with critical lower limb ischemia: ischemic rest pain, development trophic ulcers. With the development of gangrene, amputation is necessary.
3. Patients with acute ischemia: a sharp decline blood flow in the limb with the threat of gangrene.
Intravascular revascularization techniques include: balloon angioplasty, atherectomy. stent placement, thrombectomy. With the development of acute thrombosis, it is appropriate to use thrombolytic therapy within 6 hours from the moment of occlusion. Open surgical revascularization is performed by applying a bypassa vascular shunt that allows blood flow to bypass the occluded area.
